
Published on: 20/Nov/2025
Posted By: Arka Health
Vitamin D & Fertility: What the Evidence Says

The intersection of nutritional biochemistry and reproductive endocrinology has witnessed a paradigm shift in the last decade. Among the micronutrients scrutinized for their role in human fertility, Vitamin D, biologically functioning as a potent secosteroid hormone rather than a mere vitamin has emerged as a critical determinant of reproductive success. No longer confined to the realms of skeletal health and calcium homeostasis, Vitamin D is now recognized as a ubiquitous modulator of the hypothalamic-pituitary-gonadal (HPG) axis. Its influence permeates every stage of the reproductive timeline: from the recruitment of primordial follicles and the regulation of steroidogenesis to the modulation of endometrial receptivity and the maintenance of a healthy pregnancy.
This comprehensive report provides an exhaustive analysis of the current scientific literature regarding Vitamin D and fertility. It explores the molecular mechanisms by which Vitamin D exerts its effects, evaluates the clinical outcomes in natural and assisted conception, and addresses the specific epidemiological challenges faced by the Indian population. Furthermore, it outlines the integrative therapeutic protocols championed by forward-thinking institutions like Arka Anugraha Hospital, positioning the optimization of Vitamin D status not as an optional adjunct, but as a fundamental prerequisite for reproductive health.
1. The Physiology of a Secosteroid: Beyond Bone Health
To appreciate the impact of vitamin d and fertility, one must first dismantle the misconception that it is merely a nutrient required for strong bones. Biologically, Vitamin D3 (cholecalciferol) is a pro-hormone. It is synthesized in the cutaneous tissue from 7-dehydrocholesterol upon exposure to ultraviolet B (UVB) radiation. It subsequently undergoes a two-step hydroxylation process—first in the liver to form 25-hydroxyvitamin D, the major circulating form, and then in the kidney to form 1,25-dihydroxyvitamin D, the biologically active hormone known as calcitriol.
1.1 The Vitamin D Receptor (VDR) Genome
The biological plausibility of Vitamin D’s role in fertility is irrefutably established by the discovery of the Vitamin D Receptor (VDR) and the 1α-hydroxylase enzyme (CYP27B1) in reproductive tissues. Unlike other vitamins that act as cofactors for enzymes, calcitriol functions like a steroid hormone (similar to estrogen or testosterone). It crosses the cell membrane and binds to the nuclear VDR.
Upon binding, the VDR forms a heterodimer with the Retinoid X Receptor (RXR). This VDR-RXR complex translocates to the nucleus and binds to specific DNA sequences known as Vitamin D Response Elements (VDREs) located in the promoter regions of target genes. This genomic pathway allows Vitamin D to directly upregulate or suppress the transcription of thousands of genes, estimated to be roughly 3% of the human genome.
In the context of reproduction, VDRs and metabolic enzymes have been mapped extensively:
- The Ovary: VDRs are expressed in granulosa cells, theca cells, and the oocyte itself, suggesting a direct role in folliculogenesis and steroid hormone production.
- The Uterus: The endometrium expresses VDRs, and their density fluctuates across the menstrual cycle, peaking during the implantation window. This suggests Vitamin D regulates endometrial receptivity.
- The Placenta: The placenta is a major extra-renal site of Vitamin D conversion, capable of synthesizing its own active calcitriol to regulate immune tolerance and calcium transfer to the fetus.
- The Pituitary Gland: VDR presence here implies a regulatory role in the secretion of gonadotropins like Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH).
1.2 Non-Genomic Signaling Pathways
Beyond the slow, genomic regulation of gene transcription, Vitamin D also exerts rapid, non-genomic effects. These occur within seconds to minutes and are mediated by membrane-bound VDRs (mVDR). This pathway is particularly relevant for gamete physiology. For instance, in human sperm, the rapid influx of calcium required for the acrosome reaction (the process allowing the sperm to penetrate the egg) is modulated by non-genomic Vitamin D signaling. Similarly, in ovarian granulosa cells, rapid signaling cascades involving protein kinases are triggered by calcitriol, influencing immediate cellular responses to hormonal stimuli.
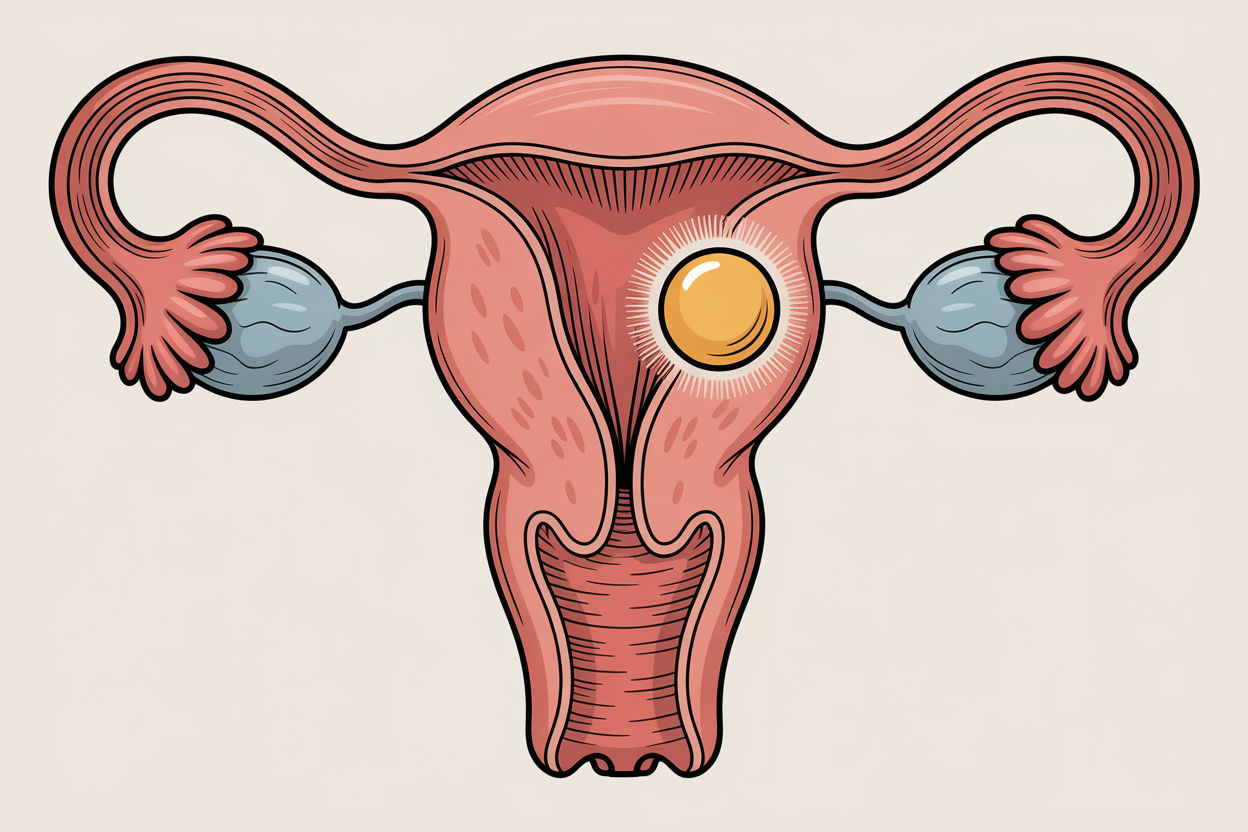
2. Ovarian Physiology: Reserve, Quality, and Folliculogenesis
The ovary is the epicenter of female fertility, and Vitamin D appears to be a crucial regulator of its function. The evidence suggests that Vitamin D status influences the ovarian reserve, the quality of the oocytes, and the hormonal environment in which they mature.
2.1 Anti-Müllerian Hormone (AMH) and the Promoter Region
Anti-Müllerian Hormone (AMH) is widely used clinically as a marker of ovarian reserve. It is produced by the granulosa cells of pre-antral and small antral follicles. The relationship between vitamin d and fertility regarding AMH is complex and rooted in genetics.
Research has identified a functional VDRE in the promoter region of the human AMH gene. This means that Vitamin D can directly stimulate the production of AMH.
- Preservation of Reserve: In women with Diminished Ovarian Reserve (DOR) or those of advanced maternal age (>40 years), studies indicate a positive correlation: higher Vitamin D levels are associated with higher AMH levels. This suggests that maintaining optimal Vitamin D may help sustain the ovarian reserve for longer.
- Seasonal Variation: The link is so potent that AMH levels in some populations exhibit seasonal fluctuations, mirroring the seasonal rise and fall of serum Vitamin D. This “seasonal” fertility may be evolutionarily conserved, ensuring conception occurs when environmental conditions (signaled by sunlight/Vitamin D) are optimal.
- The PCOS Paradox: Interestingly, in Polycystic Ovary Syndrome (PCOS), where AMH is pathologically elevated due to follicular arrest, Vitamin D supplementation has been observed to lower or normalize AMH levels. This indicates that Vitamin D acts as a homeostatic regulator—boosting low levels in DOR while curbing excessive levels in PCOS—rather than a simple stimulant.
2.2 Folliculogenesis and Steroidogenesis
Folliculogenesis is the process by which a primordial follicle matures into a dominant follicle capable of ovulation. Vitamin D influences this journey at multiple checkpoints.
- FSH Sensitivity: Vitamin D increases the sensitivity of granulosa cells to FSH. In women with vitamin d deficiency women, higher doses of exogenous gonadotropins are often required during IVF stimulation to achieve adequate follicular growth. Correcting the deficiency can restore sensitivity, leading to a more robust response with lower medication dosages.
- Progesterone Synthesis: A critical mechanism identified in animal models (specifically chicken follicles) and corroborated in human cell lines involves the enzyme CYP11A1. Vitamin D3 supplementation (10nM) significantly increases the mRNA expression of CYP11A1, the side-chain cleavage enzyme responsible for converting cholesterol into pregnenolone, the precursor to progesterone. Progesterone is the “hormone of pregnancy,” essential for maintaining the endometrium.
- Estradiol Production: Through the upregulation of the CYP19A1 (aromatase) gene, Vitamin D enhances the conversion of androgens to estrogens within the ovary. This is vital for the growth of the endometrial lining and the mid-cycle LH surge.
2.3 Oocyte Quality and Cytoplasmic Maturation
While ovarian reserve (quantity) is important, oocyte quality is paramount. The follicular fluid (FF) that bathes the developing egg contains high concentrations of Vitamin D, which correlate strongly with serum levels.
- The Glucose Connection: High-quality oocytes require significant energy. Research indicates that the metabolic profile of the follicular fluid affects oocyte competence. An imbalance, characterized by low glucose levels in the FF, correlates with poor outcomes. Vitamin D appears to modulate glucose transport and metabolism within the follicle. However, there is a nuanced “U-shaped” curve; excessive Vitamin D combined with specific glucose metabolic defects could theoretically be detrimental, though deficiency is the far more common and pressing clinical concern.
- Oxidative Stress Defense: The follicular environment is susceptible to oxidative damage, which increases with age and leads to chromosomal aneuploidy. Vitamin D exerts antioxidant effects, reducing the accumulation of Advanced Glycation End-products (AGEs) in the follicle. By mitigating oxidative stress, Vitamin D supports proper spindle formation and cytoplasmic maturation, directly impacting egg quality and fertilization potential.
Table 1: Impact of Vitamin D on Key Ovarian Markers
Marker | Effect of Vitamin D Sufficiency | Biological Mechanism | Clinical Implication |
AMH (DOR) | Maintenance / Increase | VDRE binding on AMH gene promoter. | May extend the fertile window in older women. |
AMH (PCOS) | Normalization (Decrease) | Downregulation of AMHR-II expression. | Restores ovulation and reduces cyst formation. |
FSH | Reduction / Stabilization | Enhanced ovarian sensitivity to FSH. | Lowers drug requirement for IVF stimulation. |
Progesterone | Increased Synthesis | Upregulation of CYP11A1 and 3B-HSD enzymes. | Supports luteal phase and early pregnancy maintenance. |
AGEs | Reduction | Antioxidant activity in follicular fluid. | Improves egg quality and reduces DNA fragmentation. |
3. Pathologies of Deficiency: PCOS, Endometriosis, and Fibroids
Vitamin D deficiency is not merely a passive bystander in reproductive disorders; it is an active contributor to their pathogenesis. The anti-inflammatory, metabolic, and anti-proliferative properties of Vitamin D make it a crucial therapeutic agent in managing conditions like PCOS and endometriosis.
3.1 Polycystic Ovary Syndrome (PCOS)
PCOS is the most prevalent endocrine disorder in women of reproductive age, affecting up to 15% of the population. It is characterized by ovulatory dysfunction, hyperandrogenism, and metabolic abnormalities. Vitamin d deficiency women with PCOS represents a significant subgroup with exacerbated symptoms.
- The Insulin Resistance Link: Insulin resistance (IR) is a core driver of PCOS. VDRs are present on pancreatic beta-cells, and Vitamin D is essential for insulin synthesis and secretion. Deficiency impairs insulin signaling, leading to compensatory hyperinsulinemia.
- The SHBG-Androgen Axis: Hyperinsulinemia signals the liver to decrease the production of Sex Hormone Binding Globulin (SHBG). SHBG normally binds to testosterone, rendering it inactive. When SHBG drops, free testosterone levels rise, causing hirsutism, acne, and follicular arrest. Vitamin D supplementation improves insulin sensitivity, which in turn raises SHBG levels and lowers free androgens, addressing the root hormonal imbalance.
- Metabolic Syndrome and Inflammation: Women with PCOS often exhibit chronic low-grade inflammation (elevated CRP) and dyslipidemia. Vitamin D has potent anti-inflammatory effects. Supplementation has been shown to reduce CRP levels and improve lipid profiles, creating a metabolic environment more conducive to ovulation.
- Clinical Outcomes: In PCOS patients undergoing ovulation induction or IVF, those with sufficient Vitamin D levels show higher ovulation rates and better response to Clomiphene Citrate or Letrozole compared to deficient counterparts.
3.2 Endometriosis
Endometriosis is an estrogen-dependent, chronic inflammatory condition where endometrial-like tissue grows outside the uterus. It is a leading cause of infertility and pelvic pain.
- Immunomodulation: The immune system in endometriosis patients fails to recognize and clear the ectopic tissue. Vitamin D is a potent immunomodulator. It suppresses the proliferation of T-helper 17 (Th17) cells and reduces the secretion of pro-inflammatory cytokines like Interleukin-17 (IL-17) and TNF-alpha. In animal models, Vitamin D administration (specifically at doses equivalent to 24 IU/kg) resulted in a significant reduction in the size of endometriotic lesions and lower IL-17 expression.
- Epidemiological Inverse Correlation: Large population-based studies have consistently shown an inverse correlation: women with higher serum 25(OH)D levels have a significantly lower risk of developing endometriosis (OR 0.73). Conversely, severe deficiency is associated with more advanced stages of the disease.
- Pain Management: While results are mixed, the anti-inflammatory action of Vitamin D offers a potential adjunctive therapy for the dysmenorrhea and chronic pelvic pain associated with endometriosis, potentially reducing the reliance on analgesics.
3.3 Uterine Fibroids (Leiomyomas)
Uterine fibroids are benign tumors that can interfere with implantation and cause miscarriage. Research indicates that VDR expression is downregulated in fibroid tissue compared to normal myometrium. In vitro studies demonstrate that Vitamin D inhibits the proliferation of fibroid cells and reduces the expression of extracellular matrix proteins (collagen, fibronectin) that make up the bulk of the tumor. This suggests that maintaining optimal Vitamin D levels may prevent fibroid growth or recurrence after myomectomy.
4. Male Factor Infertility: The Forgotten Half
While often focused on the female partner, fertility is a dual equation. Vitamin D receptors are abundant in the male reproductive tract, including the Leydig cells (testosterone production), Sertoli cells (sperm production), and the sperm itself.
- Sperm Motility and Capacitation: The neck and head of the sperm cell contain VDRs. Vitamin D is involved in the production of ATP (energy) within the sperm mitochondria, which is essential for motility. Furthermore, the non-genomic action of Vitamin D regulates calcium influx into the sperm, a trigger required for the acrosome reaction—the enzymatic release that allows the sperm to penetrate the egg’s outer shell.
- Testosterone Synthesis: Cross-sectional studies have shown a positive correlation between serum 25(OH)D and total testosterone levels. Men with deficiency often have lower testosterone and higher SHBG, leading to reduced bioavailable androgen. Supplementation in deficient men has been shown to boost testosterone levels, potentially improving libido and spermatogenesis.
Sperm DNA Integrity: Oxidative stress damages sperm DNA, leading to fragmentation. High DNA fragmentation is a common cause of recurrent miscarriage and IVF failure. Vitamin D’s role as an antioxidant in the seminal plasma helps protect sperm chromatin integrity during its journey through the reproductive tract.
5. Assisted Reproductive Technology (ART) & IVF Outcomes
In the high-stakes environment of In Vitro Fertilization (IVF), where emotional and financial costs are immense, optimizing every variable is critical. Vitamin D status has transitioned from a “person of interest” to a “key suspect” in IVF failure analysis.
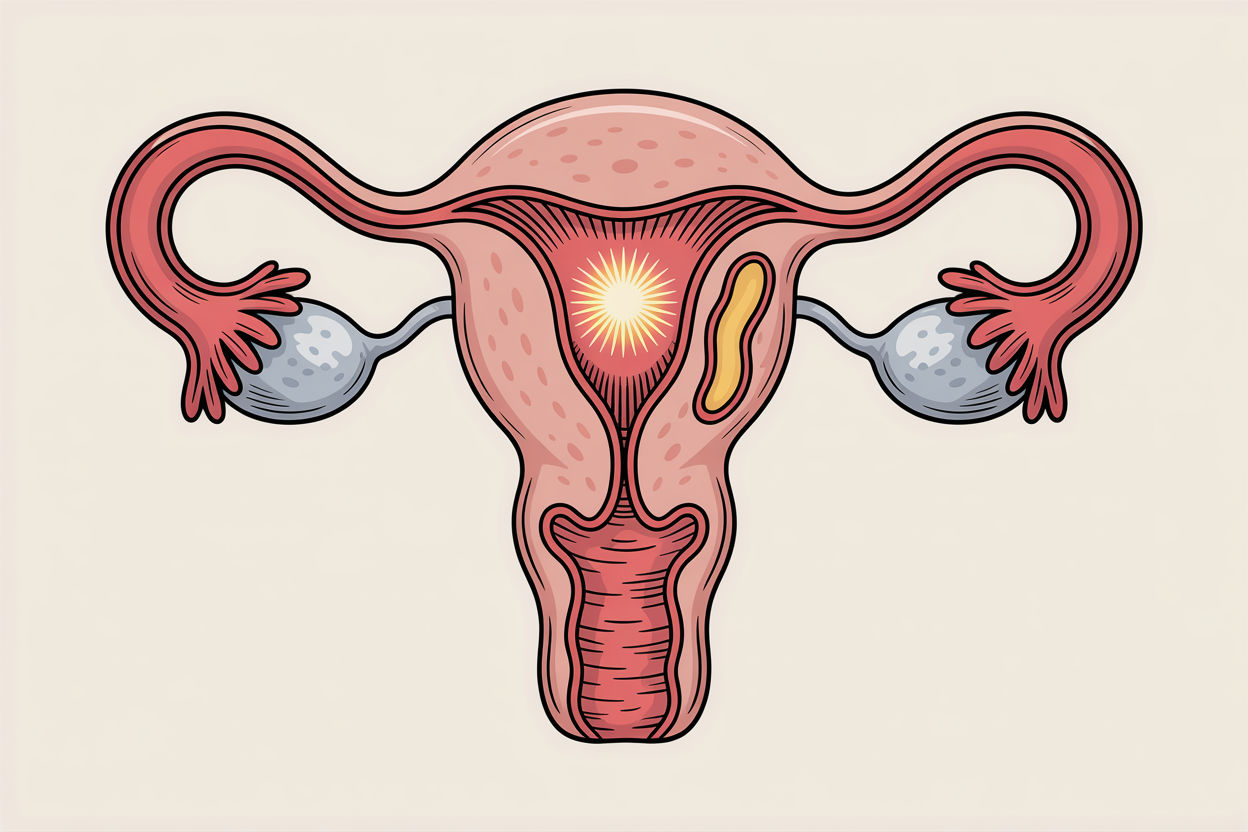
5.1 Implantation and Endometrial Receptivity
Even the highest quality embryo cannot implant in a hostile endometrium. The “window of implantation” is regulated by a cascade of genes, most notably HOXA10. Vitamin D upregulates HOXA10 expression in human endometrial stromal cells. Deficiency leads to aberrant expression of this gene, potentially rendering the endometrium non-receptive.
Furthermore, the maternal immune system must undergo a shift to “tolerate” the embryo, which is genetically distinct (semi-allogeneic). Vitamin D promotes this tolerance by shifting the immune response from a pro-inflammatory Th1 dominance to a more tolerant Th2 phenotype. This prevents the maternal immune system from attacking the implanting embryo.
5.2 The Data: Meta-Analyses and Clinical Trials
The correlation between Vitamin D and IVF success is one of the most robust findings in recent literature.
- Live Birth Rates: A recent meta-analysis and systematic review (2014-2024) confirmed that women with adequate Vitamin D levels (>30 ng/mL) have significantly higher clinical pregnancy and live birth rates compared to those who are deficient.
- Donor Egg Cycles: A pivotal study looked at women receiving donor eggs. Since the egg quality was controlled (young, healthy donors), any difference in success rates would be attributable to the recipient’s uterus. The study found that recipients with normal Vitamin D levels had significantly higher pregnancy rates than those with low levels. This isolates the benefit of Vitamin D specifically to the endometrium and implantation environment.
- DOR Subgroup Specifics: The impact is most profound in vulnerable populations. In a study of women with Diminished Ovarian Reserve (DOR), Vitamin D deficiency was associated with a drastically lower biochemical pregnancy rate (Odds Ratio 0.27) and clinical pregnancy rate (Odds Ratio 0.36). For these women, every follicle counts, and Vitamin D deficiency appears to be a catastrophic multiplier of risk
PCOS and IVF: In PCOS patients, adequate Vitamin D levels were associated with a lower risk of Ovarian Hyperstimulation Syndrome (OHSS) and higher fertilization rates, suggesting a protective metabolic effect during stimulation.
6. Pregnancy, Miscarriage, and Fetal Programming
The role of Vitamin D does not end at conception. It is vital for the maintenance of pregnancy and the long-term health of the offspring.
6.1 Miscarriage and Recurrent Pregnancy Loss (RPL)
Recurrent miscarriage is often linked to immunological rejection or chromosomal abnormalities. As discussed, Vitamin D supports the maintenance of the decidua (pregnant endometrium) and suppresses autoimmune responses that might trigger rejection. Deficiency has been identified as a risk factor for first-trimester miscarriage, particularly in women with autoimmune conditions like Antiphospholipid Syndrome.
6.2 Obstetric Complications
- Preeclampsia: This dangerous condition involves high blood pressure and organ damage. Vitamin D promotes angiogenesis (formation of new blood vessels) in the placenta. Deficiency impairs placental development, increasing the risk of preeclampsia. Supplementation (4,000 IU/day) has been shown to significantly reduce this risk.
- Gestational Diabetes (GDM): Given its role in insulin sensitivity, it is unsurprising that Vitamin D deficiency is a strong predictor for developing GDM. Maintaining levels >30 ng/mL helps regulate maternal glucose metabolism.
- Preterm Birth: Studies indicate that maintaining Vitamin D levels above 40 ng/mL is associated with a 40-60% reduction in the risk of preterm birth compared to levels below 20 ng/mL.
6.3 Fetal Programming (The Barker Hypothesis)
The effects of maternal Vitamin D status extend into the next generation. The “Barker Hypothesis” posits that the intrauterine environment programs the fetus for life.
- Bone Mineralization: Maternal deficiency leads to neonatal hypocalcemia and poor bone density (congenital rickets).
- Immune System Development: Adequate maternal Vitamin D (4,000 IU/day) has been linked to a reduced risk of atopic eczema and asthma in offspring during the first years of life.
Neurodevelopment: Emerging evidence suggests a link between severe maternal deficiency and an increased risk of autism spectrum disorders and schizophrenia in the child, highlighting the role of Vitamin D in fetal brain development.
7. The Indian Context: A Paradox of Plenty
India presents a unique and troubling public health paradox. Despite being a tropical nation with abundant sunshine, vitamin d deficiency women in India is epidemic. Studies estimate prevalence rates between 70% and 95% in the general population, with women of reproductive age being severely affected.1 This has massive implications for fertility clinics operating in India, such as Arka Anugraha Hospital.
7.1 The Melanin Barrier
The primary source of Vitamin D is cutaneous synthesis. However, melanin-the pigment responsible for darker skin tones-acts as a natural sunscreen. It competes with 7-dehydrocholesterol for UVB photons. An individual with Fitzpatrick skin type IV or V (common in India) requires 3 to 6 times more sun exposure to synthesize the same amount of Vitamin D as someone with fair skin (Type I or II). Given the cultural avoidance of sun tanning and the extreme heat preventing midday exposure, most Indian women do not achieve this threshold.
7.2 The Dietary Deficit (Vegetarianism and Phytates)
The typical Indian diet is rich in grains but poor in natural Vitamin D sources.
- Vegetarianism: Vitamin D3 is naturally found in fatty fish (salmon, mackerel), cod liver oil, and organ meats—foods largely absent from the vegetarian or lacto-vegetarian diets prevalent in India.
- Phytates: Indian diets are high in phytates (found in unleavened breads like roti, legumes, and pulses). Phytates bind to calcium and can interfere with the metabolism of Vitamin D and bone mineralization, exacerbating the effects of deficiency.
- Lack of Fortification: Unlike Western nations where milk and cereals are mandatorily fortified, food fortification in India is voluntary and inconsistent. Even “fortified” foods often contain Vitamin D2, which is less bioavailable than D3.
7.3 Socio-Economic and Environmental Factors
- Urbanization: Urban Indian women, often working indoors, show higher deficiency rates than rural women in some studies. However, rural women also suffer due to traditional clothing that covers most of the body.
- Pollution: High levels of atmospheric pollution in Indian metros can absorb UVB radiation, effectively filtering out the wavelengths needed for Vitamin D synthesis before they reach the ground.
- Obesity: The rising “diabesity” epidemic in India further complicates matters. Vitamin D is fat-soluble and gets sequestered in adipose tissue. Obese individuals need 2-3 times higher doses to achieve the same serum levels as lean individuals.
8. Integrative Clinical Protocols: Diagnosis and Treatment

Given the compelling evidence, the management of Vitamin D must be a cornerstone of fertility treatment. However, the “one size fits all” approach of standard multivitamin supplementation is often inadequate for infertile patients. A precision medicine approach, as advocated by functional and integrative models, is required.
8.1 Accurate Diagnosis and Reference Ranges
Measuring serum 25(OH)D is the first step. While identifying rickets is easy, defining “optimal fertility” is more nuanced.
- Deficient (<20 ng/mL): Critical range. Associated with osteomalacia, muscle weakness, and severe reproductive compromise.
- Insufficient (20-30 ng/mL): Sub-optimal. While metabolic bone disease may not be present, reproductive efficiency is likely impaired.
- Optimal (30-60 ng/mL): The therapeutic target. This range is associated with maximal calcium absorption, optimal immune modulation, and the highest IVF success rates.
- Therapeutic/High (60-100 ng/mL): Often used in autoimmune protocols under medical supervision.
- Toxic (>150 ng/mL): Risk of hypercalcemia.
8.2 Supplementation Strategies: Stoss vs. Daily
To correct the efficiency rapidly, especially before an IVF cycle, different protocols are employed.
- High-Dose “Stoss” Therapy: For levels <20 ng/mL, a common protocol involves 50,000 IU of Vitamin D3 once weekly for 8 weeks. This rapid loading phase is crucial because correcting deficiency with low daily doses can take months—time that fertility patients often do not have.
- Daily Maintenance: Once levels reach >30 ng/mL, a maintenance dose of 2,000 to 4,000 IU daily is typically sufficient to sustain levels. The Endocrine Society suggests that up to 10,000 IU/day poses no risk of toxicity.
- Pregnancy Dosing: During pregnancy, continuing with 2,000–4,000 IU/day is safe and necessary to support the increased demands of the fetus and placenta.
8.3 The Critical Role of Cofactors
Vitamin D does not work in a vacuum. Integrative protocols must address the cofactors required for its metabolism to prevent imbalances.
- Magnesium: The enzymes that convert Vitamin D into its active form (25-hydroxylase and 1-alpha-hydroxylase) are magnesium-dependent. High-dose Vitamin D can deplete the body’s magnesium stores, leading to symptoms like palpitations, cramps, and anxiety. Supplementation with 200-400 mg of Magnesium (Glycinate or Citrate) is recommended alongside Vitamin D.
- Vitamin K2 (MK-7): Vitamin D increases calcium absorption. Vitamin K2 activates proteins (osteocalcin and matrix GLA protein) that direct this calcium into the bones and teeth, keeping it out of the soft tissues and arteries. Taking D3 without K2 can theoretically increase the risk of arterial calcification. A ratio of roughly 100 mcg of K2 (MK-7) for every 5,000-10,000 IU of D3 is often suggested.
- Fat Intake: Being fat-soluble, Vitamin D absorption is increased by 30-50% when taken with a meal containing fat (e.g., ghee, avocado, nuts, eggs) compared to a fat-free meal.
8.4 Dietary Sources for the Indian Vegetarian
While supplements are usually necessary to correct a deficiency, diet provides a baseline.
- Mushrooms: Certain varieties like Shiitake and Maitake, when sun-dried or UV-exposed, can provide significant amounts of Vitamin D2.
- Fortified Foods: Checking labels for fortification in milk, soy milk (tofu), and orange juice is a practical strategy.
- Cheese and Paneer: Provide small amounts of D3 and calcium.
Table 2: Integrative Vitamin D Protocol for Fertility
Baseline Level (ng/mL) | Protocol Recommendation | Cofactors | Re-test Interval |
< 10 (Severe) | 50,000 IU weekly x 8-12 weeks | Mg (400mg), K2 (100mcg) | 3 months |
10 – 20 (Deficient) | 50,000 IU weekly x 8 weeks | Mg (300mg), K2 (100mcg) | 3 months |
20 – 30 (Insufficient) | 5,000 IU daily | Mg (200mg), K2 (100mcg) | 3-4 months |
30 – 60 (Optimal) | 2,000 IU daily (Maintenance) | Balanced Diet | 6-12 months |
> 100 (Elevated) | Pause supplementation | None | 3 months |
9. The Arka Anugraha Approach: Integrative Excellence
In the landscape of fertility treatments, where the focus is often obsessively on the gametes, the host environment—the patient’s body—is frequently overlooked. Arka Anugraha Hospital differentiates itself through a commitment to Integrative Medicine, a model that synthesizes the precision of modern reproductive endocrinology with the holistic wisdom of functional nutrition and lifestyle medicine.
9.1 Treating the Root Cause
Standard fertility protocols often rush to ovulation induction or IVF without addressing the underlying metabolic terrain. If a patient has Vitamin D deficiency, insulin resistance, and chronic inflammation, forcing ovulation may result in poor quality eggs or implantation failure. Arka Anugraha’s diagnostic philosophy emphasizes identifying these “silent” barriers. By correcting a simple Vitamin D deficiency, the clinic often observes improvements in FSH levels, better ovarian response, and even spontaneous conceptions in couples previously labeled with “unexplained infertility”.
9.2 Holistic Patient Care
The patient experience at Arka Anugraha is designed to be restorative.
- Nutritional Counseling: Patients receive guidance tailored to the Indian palate, helping them navigate vegetarian sources of essential nutrients like Vitamin D, B12, and Iron.
- Stress and Lifestyle: Recognizing that stress depletes nutrients and disrupts hormones, the integrative model incorporates stress management techniques. This holistic view aligns with patient reviews praising the hospital for avoiding “unnecessary strong medication” and focusing on the “root cause”.
- Evidence-Based Supplementation: Instead of generic prescriptions, supplementation is personalized based on serum levels, ensuring safety and efficacy.
By addressing the vitamin d and fertility link proactively, Arka Anugraha Hospital empowers patients to optimize their biological potential, turning the “waiting period” of fertility treatment into a “preparation period” for a healthy pregnancy.
10. Conclusion
The evidence is undeniable: Vitamin D is a cornerstone of reproductive health. Its influence extends far beyond bone density, regulating the delicate genetic and hormonal symphony required for conception. From the recruitment of follicles and the maturation of oocytes to the immune tolerance essential for implantation and the metabolic health of the pregnant mother, Vitamin D is omnipresent.
For the Indian population, specifically, the “Vitamin D Paradox” is a public health crisis with direct consequences for fertility. The combination of genetic predisposition (melanin), dietary limitations (vegetarianism/phytates), and environmental factors creates a perfect storm of deficiency. However, this is also a massive opportunity. Vitamin D deficiency is easily diagnosed and affordably treated.
Optimizing Vitamin D levels represents a low-cost, high-impact intervention that can significantly improve outcomes in ovulation health, egg quality, and IVF success rates. For clinicians and patients alike, vigilance regarding this “sunshine hormone” is not just a recommendation—it is a necessity for modern reproductive care.
11. Frequently Asked Questions (FAQ)
Q1: Can Vitamin D deficiency cause infertility on its own?
While deficiency alone may not cause absolute sterility, it is a major cause of “subfertility.” It impairs every stage of reproduction: it can stop ovulation (PCOS), reduce egg quality, prevent implantation, and increase miscarriage risk. Correcting it often removes a significant barrier to conception.
Q2: My doctor prescribed 60,000 IU per week. Is that safe?
Yes, this is a standard “loading dose” or “Stoss therapy” used to correct deficiencies rapidly. It is usually prescribed for 8-12 weeks, followed by a lower daily maintenance dose. It is safe when taken under medical supervision to monitor levels.
Q3: I spend time in the sun, but my levels are still low. Why?
In India, pollution can block UVB rays. Additionally, darker skin (more melanin) acts as a natural sunblock, requiring much longer exposure (30-45 minutes) than lighter skin. If you shower immediately with soap, you might wash away some of the oils where Vitamin D is synthesized (though this is debated, it’s better to wait). Finally, if you are overweight, Vitamin D gets trapped in fat cells, lowering blood levels.
Q4: Does Vitamin D improve egg quality in older women?
Yes. Vitamin D acts as an antioxidant in the follicular fluid, protecting the egg from aging-related damage and oxidative stress. Studies show it helps maintain ovarian reserve (AMH) in women over 40.
Q5: Should my husband take Vitamin D too?
Absolutely. Vitamin D receptors are found in sperm. Deficiency in men is linked to lower testosterone, reduced sperm count, and poor motility. Treating the male partner is just as important.
Q6: Which form of Vitamin D is best?
Always choose Vitamin D3 (Cholecalciferol) over D2. D3 is the form your body makes naturally and is much more effective at raising blood levels. Liquid caps or drops with a fat base (like coconut or olive oil) are often better absorbed than dry tablets.
Q7: Why does Arka Anugraha Hospital focus on Vitamin D?
Arka Anugraha believes in Integrative Medicine—treating the whole body to support fertility. By optimizing Vitamin D, they aim to improve your body’s natural response to treatment, potentially reducing the need for high doses of IVF drugs and improving your overall chance of a healthy baby.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
