Visceral Hypersensitivity: Why Your Gut Overreacts and How ARKA Anugraha Hospital Treats It

- Published on: 15/Dec/2025
- Posted By: Arka Health

Many people in Bengaluru live with digestive symptoms that never appear clearly on scans or endoscopy reports. The stomach burns even when there is no ulcer. A small meal feels heavy for hours. The upper abdomen aches without visible inflammation. The bloating grows until it feels like internal pressure. Tests come back normal but the discomfort persists.
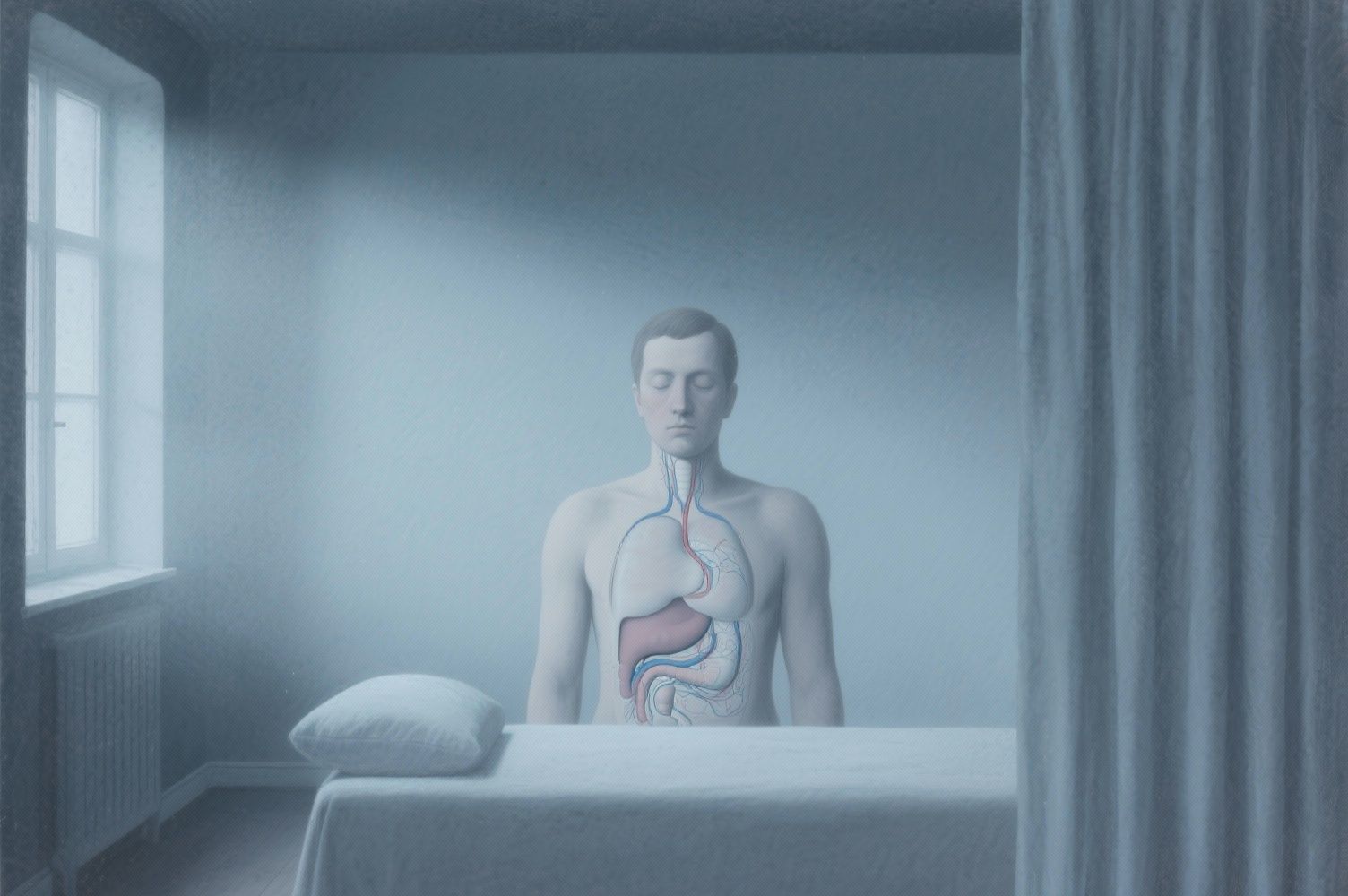
This pattern defines a condition known as visceral hypersensitivity. The nerves in the digestive tract become overly sensitive and begin to react to normal sensations as if they are painful. Visceral hypersensitivity is one of the main reasons patients develop Functional Dyspepsia, IBS-like symptoms, and chronic upper abdominal discomfort.
At ARKA Anugraha Hospital, visceral hypersensitivity is evaluated and treated through an integrative model that brings together gastroenterology, functional medicine, microbiome science, and therapies that support the gut-brain axis. Under the guidance of Dr. Gaurang Ramesh, patients receive a precise assessment followed by targeted treatment that aims to calm the nerves, restore gut integrity, and correct underlying drivers such as SIBO, post-infectious inflammation, and low-grade mucosal irritation.
This article explains why the gut becomes oversensitive, why symptoms worsen under stress, and how evidence-based treatment at ARKA helps patients recover.
What Is Visceral Hypersensitivity
Visceral hypersensitivity means the nerves inside the stomach and intestines have a lower threshold for pain. They react strongly to sensations that a healthy gut would barely notice.
There are two important components:
Hyperalgesia
A painful stimulus feels more intense than it should.
For example, gas distension is mildly uncomfortable for most people. For a person with visceral hypersensitivity, the same gas causes sharp pressure and a tight, almost gripping pain.
Allodynia
A normal sensation becomes painful.
Simple stretching of the stomach after a small meal may trigger burning or fullness because the nerves interpret it as a threat.
The gut contains more than five hundred million neurons. This complex network is known as the enteric nervous system. When these neurons become hyper-excitable, the stomach and intestines start sending amplified distress signals to the brain. This is why imaging often appears normal even when symptoms are severe.
Why Visceral Hypersensitivity Is Increasing in Urban India
Clinical patterns at ARKA Anugraha Hospital show that a large number of patients come from high-stress professional environments. Many work irregular hours, skip meals, eat quickly, or rely on processed food. This environment places constant pressure on the gut-brain axis.
Common contributing factors include:
Stress hormones like cortisol weaken the gut lining, irritate nerves, and reduce vagal tone. Low vagal tone makes the body more reactive to internal sensations.
Urban diets include more packaged foods, deep-fried snacks, gluten-rich meals, and refined sugars. These foods promote inflammation and encourage dysbiosis.
A single episode of food poisoning or stomach flu can trigger months or years of nerve hypersensitivity. This is known as post-infectious functional dyspepsia.
Microbial diversity is lower in individuals who have significant antibiotic exposure, chronic acidity medication use, or long-term stress.
Limited movement slows gastric motility and increases gas retention.
This combination explains the sharp rise in visceral hypersensitivity among Bengaluru residents, especially those managing long work hours with limited recovery time.
- What it is: Kombucha is a slightly fizzy tea drink made by fermenting tea and sugar with a culture of bacteria and yeast. It’s refreshing and available in a variety of flavors.
- How to enjoy it: Sip kombucha as a refreshing afternoon drink, but start with small amounts to see how it affects you, as it can be quite bubbly. Kombucha is a great alternative to sugary sodas, as it’s naturally low in sugar after fermentation.
The Gut-Brain Axis and Why Sensitivity Increases

The gut and brain are connected through a direct network called the gut-brain axis. The vagus nerve is the main communication pathway. It continuously transmits information about digestion, stretch, inflammation, acidity, and motility.
In a healthy state:
- The vagus nerve calms inflammation
- The brain filters unnecessary sensory signals
- The gut processes meals smoothly
In visceral hypersensitivity:
- The vagus nerve becomes less efficient due to chronic stress
- The brain amplifies sensory signals instead of modulating them
- Normal digestion feels intense or painful
This process explains why many patients feel worse during periods of emotional pressure. The gut and mind are deeply interlinked and both must be addressed for healing.
Functional Dyspepsia: How Visceral Hypersensitivity Appears Clinically

Functional Dyspepsia is one of the most common outcomes of visceral hypersensitivity. The stomach and upper small intestine send exaggerated pain signals during or after meals.
There are two main subtypes.
A. Postprandial Distress Syndrome
Key symptoms include:
- Early fullness
- Bloating immediately after meals
- Sensation of heaviness in the upper abdomen
This occurs because the upper stomach does not relax properly during eating. Pressure builds and the nerves detect this pressure as pain or discomfort.
B. Epigastric Pain Syndrome
Key symptoms include:
- Burning in the stomach area
- Sharp or gnawing pain
- Pain unrelated to structural damage
Patients often believe they have acidity or ulcers but endoscopy shows normal tissue. The burning sensation is due to acid hypersensitivity, not excess acid.
Many patients experience a mix of both subtypes.
What Triggers the Hypersensitive Response
Eosinophils and mast cells accumulate near nerves and release chemicals like histamine and serotonin. These irritants lower the pain threshold.
Commonly known as leaky gut. Stress, alcohol, NSAIDs, and dysbiosis weaken tight junctions. Undigested particles pass through and activate the immune system. This creates a continuous cycle of inflammation and nerve activation.
Even after an infection resolves, immune cells remain active and irritate the enteric nervous system.
This bacterium alters acid patterns and sensitizes receptors in the stomach lining.
Small intestinal bacterial overgrowth produces gas in areas where gas should not form. The small intestine is narrow and gas stretches it quickly. This stretch triggers pain in hypersensitive nerves.
How ARKA Anugraha Hospital Diagnoses Visceral Hypersensitivity

Diagnosis requires both structural assessment and functional testing.
Endoscopy with biopsy
Used to rule out ulcers, gastritis, tumors, and celiac changes. Biopsy may reveal subtle eosinophil clusters or H pylori not visible to the naked eye.
Hydrogen and methane breath testing
Identifies SIBO and carbohydrate malabsorption. This is one of the most useful tools at ARKA because SIBO is a frequent underlying driver of visceral hypersensitivity.
Functional laboratory markers
Tests such as secretory IgA, fecal calprotectin, and IgG food sensitivity profiles help identify inflammation, barrier damage, or immune activity.
The goal is not just to confirm functional dyspepsia but to map the root causes of the hypersensitivity.
Treatment at ARKA Anugraha Hospital: A Combined Medical and Functional Approach
ARKA uses a blended method that combines conventional gastroenterology with integrative therapies. Treatment begins by stabilising symptoms and progresses to long-term healing of the nerve pathways and gut lining.
Proton Pump Inhibitors
Useful for patients with epigastric burning. They decrease acid exposure to sensitive nerve endings but are not suitable for long-term use because they may promote SIBO.
Prokinetics
Acotiamide, Mosapride, Levosulpiride support gastric relaxation and motility. They are especially beneficial for the postprandial distress subtype.
Neuromodulators
Low-dose tricyclic antidepressants calm pain transmission through the gut-brain axis. They are not prescribed for depression in this setting but for nerve modulation.
This is a structured sequence used for long-term recovery.
Remove
Clear SIBO, treat H pylori, reduce inflammatory foods, and eliminate unnecessary medications that irritate the gut lining.
Replace
Support digestion with enzymes and, when appropriate, acid support through betaine HCl. This reduces fermentation and decreases pressure in the intestines.
Reinoculate
Probiotics are selected based on tolerance. Lactobacillus reuteri reduces pain. Saccharomyces boulardii supports barrier integrity. PHGG is used as a gentle prebiotic that improves motility.
Repair
Nutrients such as zinc-carnosine and L-glutamine are used for mucosal repair. Soothing botanicals like marshmallow root or slippery elm can provide relief to irritated surfaces.
Rebalance
This phase strengthens the gut-brain axis. Breathwork, mindfulness, and sleep regulation help reduce nerve hyperactivity and prevent relapse.
Ozone Therapy
Medical ozone modulates inflammation and supports oxygen delivery to the gut mucosa. It also influences gut microbial balance by discouraging anaerobic bacteria. Many patients report improvement in fullness, bloating, and burning after a structured ozone program.
Acupuncture and electro-acupuncture
These therapies stimulate specific nerve pathways that influence motility and pain perception. Needling at points such as ST36 and PC6 has been shown to activate endorphin release and improve vagal function.
Prescribed Yoga Therapy
Certain postures stimulate the diaphragm and vagus nerve. Techniques such as diaphragmatic breathing and bhramari support autonomic balance. This helps reduce the over-alert state of the enteric nervous system.
Dietary Strategies for a Sensitive Gut
Diet plays a major role in visceral hypersensitivity but restrictive diets are used only temporarily.
Low-FODMAP diet
Reduces fermentable carbohydrates. This minimizes gas production and pressure inside the small intestine. It is especially effective in patients with SIBO-related hypersensitivity.
Fat intake management
High-fat meals slow gastric emptying. Patients often feel heavy or nauseated after fried food or creamy dishes. Lower fat intake improves comfort.
Nerve-supporting foods
Ginger helps with motility. Peppermint oil relaxes smooth muscle. Spirulina provides antioxidant support that may benefit nerve health.
Texture and temperature
Warm, soft, and cooked foods place less strain on digestion. Soups, khichdi, dal, and steamed vegetables often work better than raw salads.
Example of a Patient Journey at ARKA
A 28 year old software engineer from JP Nagar arrived with severe bloating, burning, and early fullness. Her endoscopy was normal and she had been told repeatedly that stress was the cause. Breath tests at ARKA confirmed methane-dominant SIBO. IgG testing revealed dairy sensitivity. The patient also had low vagal tone and poor sleep.
Her treatment plan included:
- Rifaximin for SIBO
- Acotiamide for motility
- Zinc-carnosine for mucosal healing
- Dairy elimination
- PHGG fibre
- Ozone therapy
- Prescribed yoga sessions focusing on breathwork and vagal stimulation
Within eight weeks she reported a seventy percent reduction in bloating and a complete improvement in burning. Her meals felt normal again and her anxiety around food decreased significantly.
Recovery Is Possible
Visceral hypersensitivity is not an imaginary problem. It is a measurable condition involving nerve pathways, immune signals, and the gut-brain axis. With the right diagnostic approach and a comprehensive treatment plan, the gut can be desensitised and restored.
ARKA Anugraha Hospital offers one of the most complete programs for functional gut disorders in Bengaluru. Patients benefit from advanced diagnostics, medical therapy, functional medicine, and supportive treatments such as ozone therapy, acupuncture, and yoga.
Healing requires time and structure, but long-term relief is achievable.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
