Stress, Cortisol, and Gut Inflammation: How Chronic Stress Disrupts Digestive Health

- Published on: 22/Dec/2025
- Posted By: Arka Health
Many people with chronic digestive symptoms are told that their reports do not match their test results. Endoscopy looks normal. Blood work appears acceptable. Imaging shows no obstruction. Yet symptoms persist. Bloating, reflux, abdominal pain, altered bowel habits, fatigue, and food intolerance continue despite multiple treatments.
One of the most overlooked drivers behind these presentations is chronic stress and cortisol dysregulation.
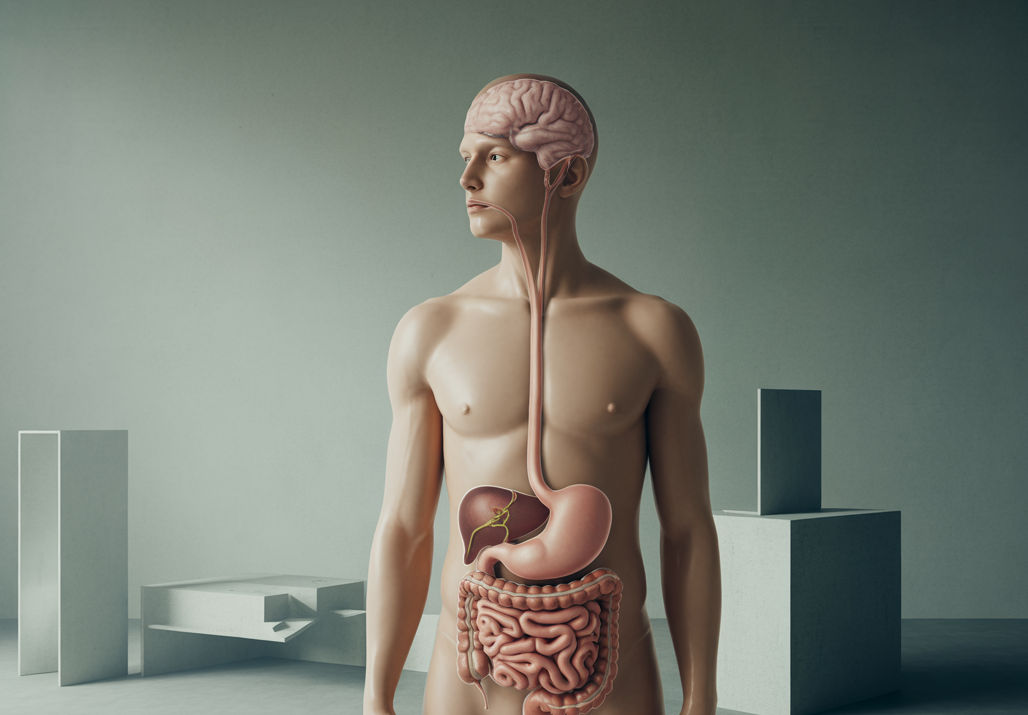
Stress does not simply affect the mind. It changes digestion at a biological level. Through the hypothalamic-pituitary-adrenal axis, stress hormones directly alter gut motility, enzyme secretion, immune activity, microbial balance, and intestinal barrier integrity. When this system remains activated long term, inflammation becomes embedded in the gut.
This article explains how stress and cortisol drive gut inflammation, why symptoms persist despite normal tests, and how recovery requires addressing both physiology and regulation.
The Stress Response and Digestive Shutdown
The human stress response evolved to protect against acute danger. When the brain perceives threat, the hypothalamus releases corticotropin-releasing hormone, activating the pituitary and adrenal glands. Cortisol is released to mobilise energy and prioritise survival.
In this state, digestion is deprioritised.
Blood flow is diverted away from the gastrointestinal tract toward muscles and the brain. Acid production in the stomach slows. Pancreatic enzymes and bile secretion are reduced. Gut movement becomes erratic or suppressed. This is appropriate for short-term stress. It becomes damaging when stress is continuous.
Modern stress is rarely physical and rarely short-lived. Work pressure, emotional load, poor sleep, unresolved trauma, and constant stimulation keep cortisol elevated for months or years. The digestive system remains in a chronic shutdown state.
Cortisol and the Breakdown of Gut Function

The Hormone Gut Connection in Chronic Bloating
High cortisol suppresses stomach acid production, pancreatic enzymes, and bile flow. Food is poorly broken down, increasing fermentation and gas formation. Low stomach acid also removes a key defence against bacterial overgrowth.
Stress disrupts coordinated gut movement. Some people develop slowed transit and constipation. Others experience urgency or diarrhoea. Many fluctuate between both, a hallmark of stress-mediated gut disorders.
Chronic stress reduces microcirculation to intestinal cells. This compromises oxygen delivery and weakens the protective mucus layer, increasing vulnerability to inflammation and permeability.
The Autonomic Nervous System and Digestive Regulation
Digestion depends on parasympathetic dominance, often referred to as the rest-and-digest state. Chronic stress locks the nervous system into sympathetic dominance.
In sympathetic overdrive:
- Gut movement becomes disorganised
- Enzyme secretion decreases
- Sphincters tighten or lose coordination
- Repair processes slow
Many patients with functional digestive disorders are not failing treatment. Their nervous system is simply not allowing digestion to function normally.
Stress, the Gut-Brain Axis, and Inflammation
The gut and brain communicate constantly through nerves, hormones, and immune signals. This bidirectional system explains why emotional stress causes digestive symptoms and why gut inflammation affects mood.
Reduced vagal tone
The vagus nerve is the primary communication pathway between the gut and brain. Chronic stress reduces vagal tone, weakening anti-inflammatory signalling and impairing gut coordination.
Neuroimmune activation
Stress activates immune cells in both the brain and the gut. Mast cells in the intestinal lining release histamine and proteases, sensitising nerves and damaging the gut barrier. This creates pain, urgency, and food reactions even without visible disease.
Intestinal Permeability and Cortisol
One of the most important consequences of chronic stress is increased intestinal permeability, often referred to as leaky gut.
Stress hormones stimulate the release of zonulin, a protein that loosens the tight junctions between intestinal cells. These junctions normally regulate what passes into the bloodstream. When they loosen, bacterial toxins and undigested food particles enter circulation.
This triggers:
- Systemic inflammation
- Immune activation
- Food sensitivities
- Fatigue and brain fog
Gut inflammation driven by stress is not confined to the digestive tract. It becomes a whole-body issue.
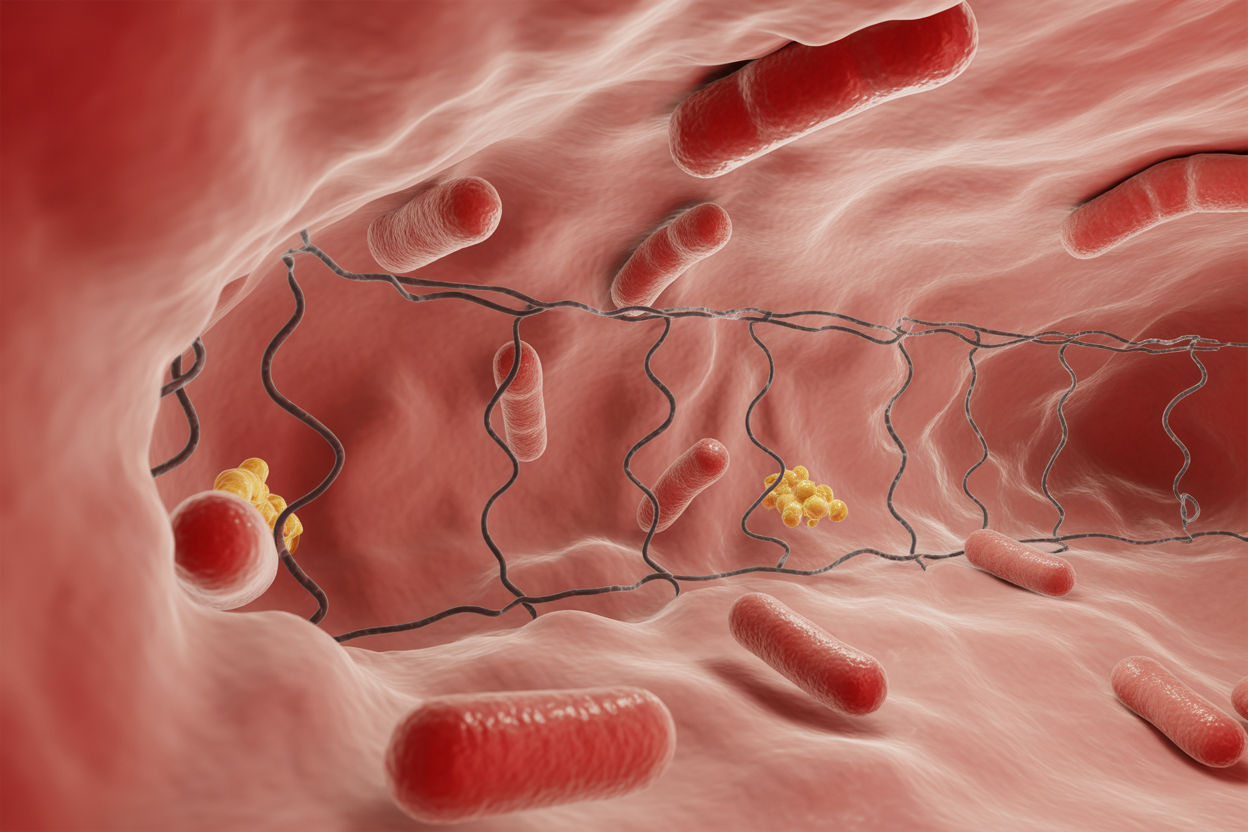
Stress-Driven Dysbiosis
Stress alters the gut microbiome directly.
Stress hormones stimulate the growth of opportunistic bacteria while suppressing beneficial species such as Lactobacillus and Bifidobacterium. Microbial diversity decreases. Short-chain fatty acid production falls. The gut loses resilience.
Behavioural changes during stress further compound this. High cortisol drives cravings for sugar and refined carbohydrates, feeding pathogenic organisms and reinforcing dysbiosis.
Over time, this creates a cycle where stress alters the microbiome, and the altered microbiome amplifies inflammation and stress signalling.
Clinical Conditions Linked to Stress-Induced Gut Inflammation

Stress and cortisol dysregulation are strongly associated with:
- Irritable bowel syndrome
- Functional dyspepsia
- Chronic bloating
- Small intestinal bacterial overgrowth
- Reflux not responding to acid suppression
- Food sensitivities without allergy
In many cases, structural disease is absent. The dysfunction lies in regulation, signalling, and immune balance.
Recovery Requires More Than Symptom Control
Suppressing acid, slowing the bowel, or masking pain does not correct stress-mediated gut dysfunction. Sustainable recovery requires restoring digestive capacity and nervous system regulation.
This typically involves:
- Supporting stomach acid and enzyme production
- Addressing microbial imbalance
- Repairing the gut barrier
- Reducing cortisol load
- Re-establishing parasympathetic dominance
Without addressing stress physiology, gut treatments often fail or relapse.
How ARKA Anugraha Hospital Approaches Stress-Related Gut Disorders
At ARKA Anugraha Hospital, stress-related gut inflammation is approached as a systems issue rather than an isolated digestive complaint.
Under the care of Dr Gaurang Ramesh, evaluation includes identifying autonomic imbalance, microbial dysbiosis, digestive insufficiency, and gut barrier dysfunction. Treatment integrates medical gastroenterology with functional and lifestyle-based interventions to restore regulation, not just suppress symptoms.
This integrative approach allows patients with long-standing unexplained digestive symptoms to move beyond repeated investigations and toward lasting recovery.
Stress does not merely coexist with gut symptoms. It actively reshapes digestion at a biological level. Cortisol alters motility, immunity, permeability, and microbial balance, creating inflammation even when conventional tests appear normal.
Understanding this connection shifts treatment away from frustration and toward resolution. When stress physiology is addressed alongside gut health, recovery becomes possible.
FAQs
1. Can stress really cause gut inflammation even if tests are normal?
Yes. Stress can disrupt gut barrier function and immune balance without causing visible damage on endoscopy or scans.
2. Why do digestive symptoms worsen during stressful periods?
Stress increases cortisol, slows digestion, reduces enzymes, and increases inflammation, all of which worsen gut symptoms.
3. Can stress cause leaky gut?
Yes. Stress hormones stimulate zonulin release, which loosens tight junctions and increases intestinal permeability.
4. Does stress affect stomach acid levels?
Chronic stress suppresses stomach acid production, leading to poor digestion, bloating, and bacterial overgrowth.
5. Why do PPIs not help stress-related reflux?
Stress-mediated reflux is often caused by motility issues and hypersensitivity rather than excess acid.
6. Can gut inflammation affect mental health?
Yes. Inflammatory signals from the gut can influence brain function, contributing to anxiety, low mood, and brain fog.
7. Is treating stress necessary for gut healing?
In stress-driven gut disorders, addressing stress physiology is essential for lasting improvement.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
