Prolotherapy Explained: How Strengthening Ligaments Resolves Chronic Pain

- Published on: 29/Jan/2026
- Posted By: Arka Health

Suresh had been living with lower back pain for nearly eight years. He had visited multiple doctors, undergone countless X-rays and MRI scans, tried physical therapy, and received several cortisone injections. Each intervention provided temporary relief at best, and some seemed to make things worse. His imaging reports always came back showing “mild degenerative changes” or “nothing significant,” yet he could barely sit through a two hour meeting without excruciating discomfort shooting down his leg. His doctors kept telling him the scans looked fine, leaving him frustrated and confused. How could he be in so much pain when the tests showed so little?
What Suresh’s doctors had missed was not visible on any static MRI. The problem was not his discs or his bones. The problem was his ligaments. These tough fibrous bands that hold his spine together had become stretched and lax, creating instability that only showed up when he moved, twisted, or bore weight. This dynamic instability was the hidden source of his years of suffering.
This is where prolotherapy enters the picture, a regenerative treatment specifically designed to address the root cause that conventional medicine often overlooks: ligament weakness and joint instability. At ARKA Anugraha Hospital, we recognize that chronic pain is rarely just about inflammation or structural damage visible on scans. More often, it is about stability, about the integrity of the connective tissues that hold your skeleton together and allow safe, pain free movement.
Understanding the Hidden Architecture of Joint Stability
To appreciate why prolotherapy works, you first need to understand what ligaments actually do and why their failure creates such persistent problems.
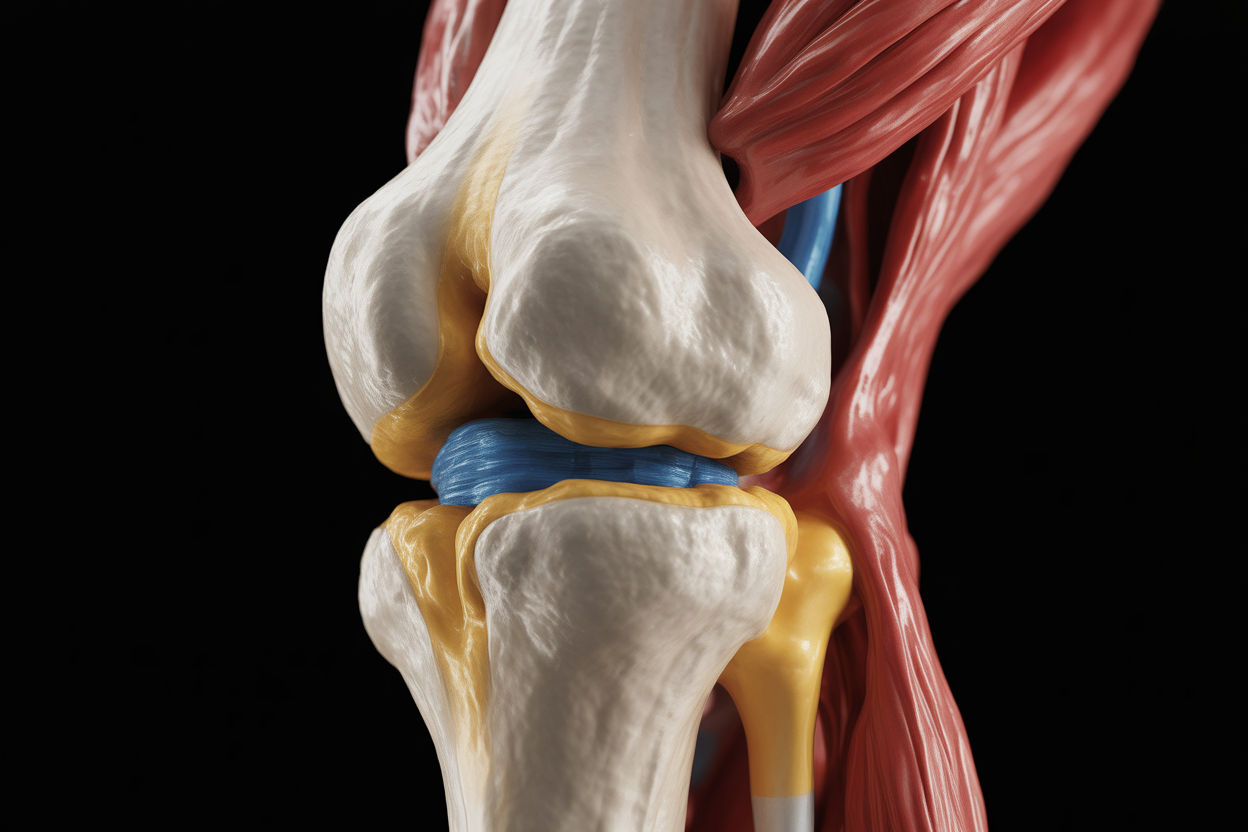
Your skeleton is not a rigid structure held together by bone alone. Instead, your body functions more like a suspension bridge, where bones act as compression elements and ligaments, tendons, and fascia act as tension elements. The ligaments are the cables that keep everything aligned and stable. When these cables become loose or damaged, the entire structure becomes unstable.
Ligaments were once thought of as simple mechanical straps, passive restraints that prevented bones from moving too far. Modern research reveals they are far more sophisticated. Ligaments are densely packed with specialized nerve endings called mechanoreceptors and proprioceptors. These sensors constantly monitor joint position, tension, and movement speed, sending real time information to your brain about where your body is in space and whether movement is safe.
When a ligament is healthy and taut, it maintains perfect joint alignment and sends reassuring signals that enable fluid, confident movement. But ligaments have a critical weakness: they have very poor blood supply compared to muscles. This means when they get stretched or torn, they often do not heal properly on their own. Unlike a muscle strain that heals in weeks, a ligament injury can remain weak indefinitely, creating chronic instability.
The Cascade of Problems From Loose Ligaments
When a ligament becomes lax, whether from a sudden injury like a car accident or from years of poor posture and repetitive stress, it triggers what specialists call the cumulative injury cycle. Understanding this cascade explains why your pain persists despite normal imaging and why treatments targeting only inflammation provide temporary relief at best.
First comes structural instability. The loose ligament allows excessive movement between the bones it is supposed to stabilize. You might feel this as a sensation of your joint giving way, slipping, or feeling unreliable. In the spine, this can mean vertebrae shifting slightly out of position during movement. In the knee, it might mean the femur sliding excessively over the tibia.
Next, your nervous system responds with protective muscle guarding. Your brain receives alarm signals from the damaged ligament’s mechanoreceptors indicating that the joint is not stable. In response, it commands the surrounding muscles to contract continuously, essentially asking them to do the stabilizing job the ligament can no longer perform. This is why you develop chronic muscle tightness and spasms that massage and stretching cannot resolve. The tight muscles are not the problem. They are your body’s desperate attempt to protect an unstable joint.
Over time, the abnormal movement patterns accelerate wear and tear on cartilage. When bones move with excessive motion or in wrong directions, they grind against cartilage surfaces in ways they were never designed to handle. This friction progressively erodes the protective cartilage, eventually showing up on X-rays as arthritis. Conventional medicine then treats the arthritis while ignoring the ligament laxity that caused it in the first place.
Finally, the shifting bones can compress nerves, creating pain that radiates far from the actual problem. This nerve compression produces numbness, tingling, and burning sensations that can mimic serious neurological conditions, leading to unnecessary and often unhelpful treatments.

The Mystery of Referred Pain: Why Your Knee Hurts When the Problem Is Your Hip
One of the most fascinating and clinically important aspects of ligament injury is referred pain. When a ligament is damaged, it rarely hurts only at the injury site. Instead, it projects pain to distant areas of your body through complex neural pathways. This phenomenon leads to countless misdiagnoses and failed treatments because doctors treat the area that hurts rather than the ligament causing the pain.
Pioneer researchers in prolotherapy mapped these referral patterns by tracking thousands of patient experiences. What they discovered was that specific ligaments consistently refer pain to predictable distant locations. For example, a loose iliolumbar ligament in your lower back commonly refers pain to your groin, inner thigh, or even genitals. Patients get worked up for hernias or urinary infections when the real problem is a spinal ligament.
Similarly, the sacroiliac ligaments in your pelvis, when lax, refer pain down the back of your thigh and into your calf and foot, perfectly mimicking sciatica from a herniated disc. Countless patients undergo back surgery for presumed disc problems when the actual culprit is pelvic ligament instability.
Even more surprising, the sacrotuberous ligament in your pelvis refers pain directly to your heel. This means someone treated endlessly for plantar fasciitis with foot stretches, orthotics, and local injections may get no relief because the source of their heel pain is actually a loose ligament in their pelvis, far from where it hurts.
Understanding these patterns is crucial at ARKA Anugraha Hospital. Our physicians are trained to recognize referred pain patterns and palpate specific ligament attachments to reproduce your exact pain, identifying the true source even when imaging appears normal.
Related service: Comprehensive musculoskeletal evaluation at ARKA Anugraha Hospital uses functional assessment and palpation techniques to identify hidden sources of chronic pain.
How Prolotherapy Actually Works: Restarting the Healing Process
Prolotherapy is elegantly simple in concept yet profound in effect. The treatment involves injecting a mild irritant solution, most commonly concentrated dextrose sugar, directly into the weakened ligament attachments where they connect to bone. This deliberate irritation restarts a healing process that had stalled or never properly completed.
The mechanism unfolds in three distinct biological phases that mirror your body’s natural response to injury.
The inflammatory phase begins immediately after injection. The concentrated dextrose solution creates what is called an osmotic shock. Because the solution outside the cells is much more concentrated than the fluid inside, water rushes out of local cells to balance the concentration. This cellular dehydration causes a small number of cells to rupture, releasing their contents into the surrounding tissue.
Your immune system interprets this as a fresh injury. White blood cells rush to the area, releasing inflammatory chemicals that clean up cellular debris and prepare the tissue for reconstruction. This is why you feel soreness and stiffness for a few days after treatment. This inflammation is not a side effect to be suppressed. It is the essential first step of healing, the wake up call that mobilizes your body’s repair systems.
The proliferative phase follows, typically lasting several weeks. The inflammatory cells release powerful growth factors including platelet derived growth factor and transforming growth factor beta. These chemical messengers activate fibroblasts, the builder cells responsible for creating new connective tissue. The fibroblasts multiply rapidly and begin secreting fresh collagen fibers. Day by day, week by week, the ligament thickens as new structural material is laid down. This is literal tissue growth, not just reduced inflammation.
The remodeling phase is the longest, extending for months. The newly formed collagen starts out disorganized, like a pile of rope thrown randomly on the ground. As you move and stress the joint normally during this phase, the collagen fibers align themselves along the lines of mechanical stress, like rope being pulled straight. Strong chemical cross links form between the fibers, giving the ligament increasing tensile strength. The end result is a ligament that is measurably thicker, stronger, and more capable of stabilizing the joint than before treatment.

Why Dextrose: The Science of Safe Stimulation
You might wonder why sugar water can trigger such powerful healing. Dextrose is chosen for specific reasons that make it ideal as a proliferant agent.
First, it is completely natural and biocompatible. Dextrose is simply glucose, a sugar your body uses constantly for energy. There is nothing foreign or synthetic about it. Once it has delivered the osmotic signal and triggered the healing cascade, it is simply metabolized through normal pathways or excreted, leaving no residue.
Second, the mechanism is purely physical and chemical, not pharmacological. Dextrose does not bind to receptors or interfere with cellular processes like drugs do. It creates a signal through osmotic pressure, triggers a response, and then disappears. This makes it remarkably safe with minimal risk of allergic reactions or unexpected interactions.
Third, the solution can be precisely adjusted. By varying the concentration from 12.5 percent to 25 percent, physicians can modulate the strength of the healing response based on the tissue being treated and the patient’s healing capacity.
The Integrative Foundation: Why Some People Heal Better Than Others
At ARKA Anugraha Hospital, we have learned that prolotherapy provides the signal to heal, but your body must have the capacity to execute that healing. This is where the integrative approach becomes essential. Two patients can receive identical prolotherapy treatments for identical injuries and have completely different outcomes. The difference often lies not in the injection but in their internal physiological environment.
Your digestive health plays a surprisingly critical role. When your gut microbiome is imbalanced and your intestinal lining becomes permeable, bacterial toxins enter your bloodstream, creating systemic inflammation. This inflammatory state keeps your fibroblasts in a constant defensive mode, unable to respond effectively when prolotherapy calls them to action. Additionally, if gut inflammation prevents proper absorption of amino acids, vitamins, and minerals, your body literally lacks the raw materials needed to build new collagen.
Hormonal balance is equally important. Thyroid hormones directly regulate the metabolic activity of fibroblasts. Low thyroid function slows their ability to proliferate and produce collagen, dramatically reducing treatment effectiveness. For women, hormones like relaxin and estrogen that fluctuate during menstrual cycles can affect ligament laxity throughout the body, which is why women are more prone to ACL tears and may require adjusted treatment protocols.
Blood sugar control cannot be overlooked. Chronic high glucose damages proteins through a process called glycation, making newly formed collagen stiff and brittle rather than strong and flexible. High blood sugar also impairs stem cell function, reducing your regenerative capacity. For diabetic patients or those with metabolic syndrome, optimizing glucose control before and during prolotherapy significantly improves outcomes.
Even psychological stress matters. Chronic stress elevates cortisol, a hormone that breaks down collagen and suppresses healing. Someone under severe ongoing stress may heal more slowly and experience more pronounced post treatment soreness.
This whole body context is why the evaluation at ARKA Anugraha Hospital goes far beyond examining the painful joint. We assess gut function, metabolic markers, hormonal status, nutritional adequacy, and stress levels to ensure your body is prepared to respond optimally to the regenerative signal prolotherapy provides.
Where Prolotherapy Shines: Common Applications
Prolotherapy can be applied virtually anywhere ligament weakness or tendon degeneration is causing pain and dysfunction. Let me walk you through some of the most common and successful applications.
For chronic lower back pain and sacroiliac joint problems, prolotherapy often succeeds where other treatments fail. Most back pain is not actually caused by herniated discs despite what MRI reports emphasize. The more common culprit is ligament laxity allowing excessive movement between spinal segments or instability in the sacroiliac joints connecting your spine to your pelvis. Prolotherapy injections into these ligaments stabilize the spine, taking pressure off nerves and eliminating the protective muscle spasms that cause so much discomfort. Clinical trials show success rates exceeding 80 percent for carefully selected patients.
Knee pain, especially osteoarthritis, responds remarkably well when ligament laxity is a contributing factor. If your medial collateral ligament or other stabilizing structures have become loose, your knee bones slide excessively during walking, grinding down cartilage and causing pain. By tightening these ligaments, prolotherapy reduces abnormal motion, protecting remaining cartilage and often eliminating pain even when X-rays show moderate arthritis.
Chronic neck pain and headaches often stem from ligament injuries in the cervical spine, particularly common after whiplash accidents. Loose ligaments allow vertebrae to shift, irritating nerves and blood vessels. This can cause not just neck pain but also headaches, dizziness, ringing in the ears, and facial pain. Strengthening the posterior neck ligaments and facet joint capsules restores stability and resolves this constellation of symptoms.
Shoulder problems including rotator cuff weakness and instability benefit from prolotherapy to the tendon insertions and supporting ligaments. Rather than surgically cutting or shaving tissue, prolotherapy strengthens the attachments, allowing the rotator cuff to function properly and preventing the upward migration of the shoulder bone that causes impingement and bursitis.
Tennis elbow, golfer’s elbow, and other chronic tendon conditions are classic prolotherapy indications. These conditions represent tendon degeneration at the attachment to bone, not active inflammation. Because there is no inflammation, anti inflammatory medications do not work. Prolotherapy converts the stagnant degenerative state back into active healing, resolving problems that may have persisted for years.
Read next: Understanding chronic tendon pain and regenerative treatment options at ARKA Anugraha Hospital.
Prolotherapy Versus Cortisone: A Critical Distinction
If you have chronic pain, you have likely been offered cortisone injections. Understanding the fundamental difference between cortisone and prolotherapy is crucial for making informed treatment decisions.
Cortisone is catabolic, meaning it breaks down tissue. It works by powerfully suppressing your immune system and blocking inflammation. This stops pain quickly, which can be valuable in acute situations. However, cortisone also inhibits collagen synthesis and weakens connective tissue. Studies have documented that repeated cortisone injections thin cartilage, weaken tendons, and significantly increase the risk of tendon rupture. Cortisone offers temporary symptom relief while potentially accelerating the underlying degeneration.
Prolotherapy is anabolic, meaning it builds tissue. Rather than suppressing healing, it stimulates it. While relief may take longer to appear because you are waiting for actual tissue to grow, the results are structural and lasting. Comparative studies consistently show that while cortisone may provide better relief at two weeks, prolotherapy delivers far superior outcomes at three months, six months, and one year. Patients receiving cortisone often return to baseline pain or worse, while those receiving prolotherapy maintain steady improvement.
This distinction is not just academic. If you have ligament laxity causing your pain, cortisone will make you feel better temporarily while your ligaments continue weakening, setting you up for eventual treatment failure or surgery. Prolotherapy addresses the structural problem, potentially preventing the need for surgery altogether.

Your Treatment Journey: What to Expect
Understanding what happens during prolotherapy treatment helps reduce anxiety and sets realistic expectations.
Your initial visit involves detailed evaluation. The physician takes a comprehensive history, performs a physical examination focusing on joint stability and ligament palpation, and reviews any imaging you have had. Importantly, they assess your overall health including digestive function, hormonal status, and nutritional adequacy to ensure you are prepared to heal effectively.
The injection procedure itself is performed in the office and typically takes 20 to 40 minutes depending on how many sites need treatment. The skin is cleaned thoroughly with antiseptic. Using precise anatomical knowledge, the physician injects the dextrose solution mixed with local anesthetic directly into the ligament and tendon attachments where they connect to bone. Multiple injections are usually given in a single session to treat the entire unstable joint complex.
Most patients describe the sensation as brief pinching or pressure. The local anesthetic in the solution numbs the area within seconds, making the remainder of the procedure comfortable. Some areas like the spine or pelvis may be guided by ultrasound or fluoroscopy for precision and safety.
After treatment, you will feel numbness initially from the anesthetic, followed within hours by a sensation of soreness, stiffness, or fullness in the treated area. This is the inflammation beginning, which means healing has started. This soreness typically peaks around day two or three and then gradually subsides over the following days. It is described as a deep, achy feeling rather than sharp pain, similar to how muscles feel after a hard workout.
Movement is encouraged during recovery. Gentle walking and normal daily activities help the new collagen fibers align properly. However, high impact activities, heavy lifting, or sports should be avoided for about a week after each treatment. The key is movement without excessive stress.
One critical instruction: avoid anti inflammatory medications. Do not take ibuprofen, naproxen, aspirin, or other NSAIDs for at least 7 to 10 days before and after treatment. These drugs work by blocking the very inflammatory pathways prolotherapy uses to trigger healing. Taking them essentially neutralizes your treatment. Simple pain relievers like paracetamol are fine if you need them.
Most conditions require a series of treatments rather than a single injection. The typical protocol involves three to six sessions spaced four to six weeks apart. This timing matches the natural biological timeline of collagen synthesis and maturation. Each session builds upon the layer of tissue deposited by the previous one. Many patients notice progressive improvement, with the most dramatic changes often appearing after the third or fourth treatment.
Safety Considerations and Who Should Not Receive Prolotherapy
Prolotherapy has an excellent safety record when performed by trained practitioners, but certain situations require special consideration.
The treatment should not be performed if you have an active infection in or near the joint, an acute fracture that needs immobilization, or severe unmanaged bleeding disorders. Patients taking high dose immunosuppressive medications for autoimmune conditions may not mount the necessary healing response, making prolotherapy less effective.
The most common experience after treatment is temporary soreness lasting a few days. Minor bruising at injection sites is possible. Serious complications like nerve injury or pneumothorax are extremely rare and almost always result from practitioner inexperience rather than inherent risks of the procedure.
Because prolotherapy relies on your body’s healing capacity, conditions that impair healing require special attention. Uncontrolled diabetes, severe malnutrition, or advanced age with frailty may reduce treatment effectiveness, though they are not absolute contraindications. This is why the integrative evaluation at ARKA Anugraha Hospital is so important. By optimizing your metabolic health, nutritional status, and inflammatory load before beginning treatment, we maximize your chances of excellent outcomes.
Beyond the Injection: Supporting Your Healing
Prolotherapy works best when supported by proper nutrition. Your body cannot build new tissue without raw materials. During your treatment course, focused nutritional support significantly enhances outcomes.
Vitamin C is absolutely essential. This vitamin is required for a critical step in collagen formation called hydroxylation. Without adequate vitamin C, the collagen your body produces will be weak and defective. Supplementing with 1000 to 2000 milligrams daily during treatment is standard protocol.
Protein intake matters because collagen is protein. If your diet is protein deficient, you lack the amino acid building blocks for tissue construction. Aim for high quality protein sources or consider collagen peptide supplements that provide the specific amino acids ligaments need in their exact proportions.
Certain minerals act as cofactors in healing. Zinc is essential for DNA synthesis and cellular division during the proliferative phase. Manganese activates enzymes that form the structural matrix of connective tissue. Ensuring adequate intake of these trace minerals supports optimal healing.
Proper hydration is often overlooked but important. The healing processes occur in the aqueous environment of your tissues. Dehydration can slow the biological reactions necessary for collagen synthesis and maturation.
Making Your Decision
If you are struggling with chronic pain that has not responded to conventional treatments, if your imaging looks relatively normal despite severe symptoms, or if you have been told you need surgery but want to explore less invasive options first, prolotherapy deserves serious consideration.
The ideal candidate has pain driven by joint instability or ligament laxity rather than severe structural damage requiring surgical repair. You need reasonable overall health and the willingness to commit to a series of treatments spaced over several months. You must be able to avoid anti inflammatory medications during treatment and follow post injection activity guidelines.
At ARKA Anugraha Hospital, prolotherapy is not offered as a standalone miracle cure but as part of a comprehensive regenerative strategy. We address the whole person, optimizing gut health, metabolic function, hormonal balance, and nutritional status to create the ideal internal environment for healing. This integrative approach transforms a simple injection technique into a powerful pathway to lasting recovery.
For patients like Suresh, whose story opened this article, prolotherapy finally addressed the root cause conventional medicine had missed. After completing a series of four treatments over five months, his ligaments regained their strength, his spine stabilized, and his eight year battle with chronic back pain resolved. He returned not just to work but to playing cricket with his son, an activity he thought he had lost forever.
Your chronic pain does not have to be a life sentence. When the problem is instability rather than irreversible damage, when the ligaments that hold you together have simply become too loose to do their job, prolotherapy offers a path back to stability, strength, and pain free movement. The treatment works with your body’s own healing wisdom, providing the signal and support for genuine structural repair rather than temporary symptom suppression.
FREQUENTLY ASKED QUESTIONS
- How is prolotherapy different from prolozone therapy offered at ARKA Anugraha Hospital? Prolotherapy uses concentrated dextrose sugar solution to create controlled inflammation that stimulates ligament repair and collagen growth. Prolozone combines dextrose with medical ozone gas for additional mitochondrial stimulation and oxygenation. Both are regenerative treatments but work through slightly different mechanisms. Your physician determines which is most appropriate based on your specific condition, with prolotherapy often preferred for pure ligament laxity.
- Why do my MRI and X-ray reports show nothing wrong when I have severe chronic pain? Standard imaging captures your joints in static positions while lying still. Ligament laxity is a dynamic problem that only appears during movement, weight bearing, or specific positions. Additionally, early ligament injuries involve microscopic fiber disruption and collagen disorganization that standard MRI resolution cannot detect. This is why palpation examination and functional testing are essential for accurate diagnosis.
- How many prolotherapy treatments will I need before experiencing pain relief? Most patients require three to six treatment sessions spaced four to six weeks apart. This timing allows your body to complete each healing phase before the next stimulation. Some people notice improvement after two sessions, while complex instability patterns may require more. Relief builds progressively as each treatment adds another layer of strengthened tissue. Maximum benefit typically appears three to six months after completing the series.
- Why must I avoid ibuprofen and other anti inflammatory medications during prolotherapy? Prolotherapy works by deliberately creating inflammation to trigger healing. Anti inflammatory medications like ibuprofen, naproxen, and aspirin block the cyclooxygenase enzymes that produce the inflammatory signals your body needs for tissue repair. Taking these drugs during treatment essentially neutralizes the therapy by preventing the healing cascade from activating. Simple pain relievers like paracetamol are safe alternatives.
- Can prolotherapy fix a herniated disc or do I still need surgery? Prolotherapy cannot physically shrink or remove a herniated disc. However, most pain from disc herniations actually results from spinal instability allowing excessive movement that irritates nerves. By strengthening the ligaments stabilizing your vertebrae, prolotherapy often eliminates pain even though the disc bulge remains visible on imaging. Many patients avoid surgery this way, though severely ruptured discs with progressive neurological deficits still require surgical evaluation.
- How does prolotherapy compare to cortisone injections my previous doctor recommended? Cortisone and prolotherapy work in opposite ways. Cortisone suppresses inflammation and immune response, providing rapid pain relief but weakening tissue over time and preventing healing. Prolotherapy stimulates inflammation and immune activity to build new, stronger tissue. Studies show cortisone provides better relief at two weeks but prolotherapy delivers superior outcomes at six to twelve months. For chronic conditions involving tissue weakness, prolotherapy addresses the root cause.
- Why does ARKA Anugraha Hospital assess my gut health and nutrition for joint pain? Your body needs specific nutrients to build collagen and requires a low inflammatory state for effective healing. Gut dysbiosis and intestinal permeability create systemic inflammation that keeps fibroblasts defensive rather than regenerative. Poor nutrient absorption means your body lacks the amino acids, vitamins, and minerals needed for tissue construction. Optimizing gut health and nutritional status ensures prolotherapy signals produce maximal healing rather than weak, inadequate tissue.
- What can I do to maximize my results from prolotherapy treatment? Maintain adequate protein intake and supplement with vitamin C, zinc, and collagen peptides during treatment. Avoid anti-inflammatory medications for 7 to 10 days before and after each session. Stay well hydrated and keep moving gently without high impact activities for the first week. Address underlying metabolic issues like blood sugar control and thyroid function. Following these guidelines creates optimal conditions for strong, lasting tissue regeneration.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
