Prolotherapy for Hip Pain: Strengthening Ligaments When Your Joint Feels Unstable

- Published on: 27/Jan/2026
- Posted By: Arka Health

Meena’s hip pain started subtly at age 54. The Bangalore homemaker noticed her right hip felt loose when climbing stairs, as if her leg might give way. Within months, the vague instability transformed into constant deep aching in her groin and outer hip. Standing to cook meals became unbearable. Getting up from sitting required pushing off with her arms. Her limp was so pronounced that her grandchildren asked why she walked funny.
Her orthopedist’s X-rays showed mild osteoarthritis with slight joint space narrowing. The prescription was predictable: anti inflammatory medications, physical therapy, and glucosamine supplements. When those failed after four months, a corticosteroid injection provided six weeks of relief before pain returned worse than before. At her follow up, her doctor explained that her arthritis would progressively worsen, eventually requiring total hip replacement. At 54, Meena faced the prospect of major surgery within years, permanently altering her hip joint.
When Meena learned about prolotherapy at ARKA Anugraha Hospital, she discovered something her previous doctors never mentioned: her hip pain stemmed not primarily from cartilage wear but from ligament laxity. The strong ligaments normally stabilizing her hip joint had stretched and weakened, allowing excessive motion that created the giving way sensation and grinding forces on remaining cartilage. Her muscles worked constantly trying to compensate for failed ligaments, causing the chronic deep ache and fatigue.
After five prolotherapy sessions over five months, Meena’s transformation was remarkable. The instability vanished. She could climb stairs confidently, stand cooking for hours, rise from chairs normally, and walk without limping. Four years later, she remains active with her grandchildren, her hip having genuinely stabilized rather than just temporarily numbed. Surgery has been indefinitely postponed through actual ligament repair.

Why Your Hip Pain Is Really About Loose Ligaments Not Just Worn Cartilage
Understanding why prolotherapy succeeds for hip pain requires recognizing that chronic hip discomfort rarely stems solely from cartilage erosion. The prevailing medical narrative focuses on osteoarthritis as mechanical wear and tear where bone eventually grinds on bone. However, this explanation fails to account for why many patients with severe cartilage loss on X-rays experience minimal pain while others with mild changes suffer debilitating symptoms.
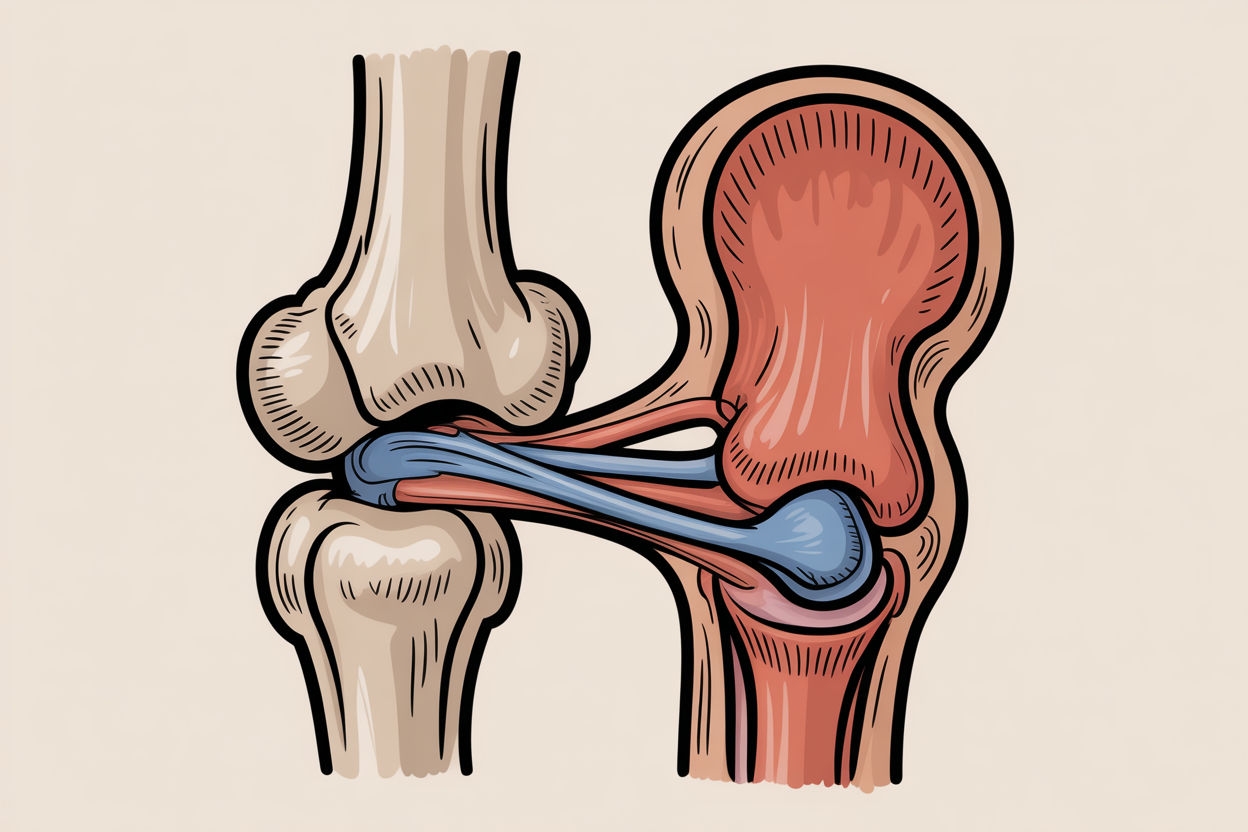
The hidden culprit in most chronic hip pain is ligament laxity, also called joint instability. Your hip functions as a tensegrity structure where stability depends not just on bone fitting together but on continuous tension from the soft tissue network surrounding it. Three major ligaments encasing your hip joint provide the static stability preventing excessive motion.
The iliofemoral ligament, shaped like an inverted Y on the front of your hip, is the strongest ligament in your entire body. It prevents hyperextension and supports your upper body weight every time you stand or walk. Chronic poor posture creating swayback, repetitive hip extension from running or yoga, or prolonged sitting that shortens and weakens this tissue leads to micro tearing and progressive laxity. Pain from iliofemoral looseness manifests as deep groin aching frequently misdiagnosed as hip flexor strain.
The pubofemoral ligament reinforces the front and bottom of your hip capsule, preventing excessive leg abduction and extension. Injury occurs during sports involving lateral movements or splits. Weakness here contributes to groin pain and instability during walking. The ischiofemoral ligament situated on your hip’s back side limits internal rotation and adduction. Laxity here allows your femoral head to shift backward, potentially impinging on your sciatic nerve creating symptoms mimicking sciatica though the root cause remains capsular instability.
These ligaments are not merely mechanical ropes but sophisticated sensory organs densely innervated with mechanoreceptors providing proprioception, your brain’s ability to sense joint position. Healthy ligaments detect strain and immediately signal surrounding muscles to contract stabilizing the joint. When ligaments become lax, this signaling delays or fails entirely. Your muscles do not fire in time to protect the joint, leading to uncoordinated movement, micro trauma to cartilage, and the sensation of your leg giving way.
Related service: Comprehensive biomechanical hip evaluation at ARKA Anugraha Hospital determines if your pain stems from ligament laxity requiring regenerative treatment rather than just cartilage wear.
The Degenerative Cascade When Ligaments Fail
Once your primary hip stabilizers become compromised, your joint enters a destructive cycle called the degenerative cascade. Micro instability begins as your femoral head moves excessively within the acetabulum socket. This movement is often too subtle to detect on static MRI but devastating to joint function. Instead of smooth gliding motion, your articular cartilage experiences shear forces, grinding sideways rather than compressing straight down.
Cartilage is brilliantly designed to handle compression but fails under shear stress. Under constant grinding, cartilage begins to fibrillate and wear away. This marks osteoarthritis onset, but the arthritis is a consequence not the cause. Your body attempting to stabilize the wobbly joint grows extra bone at margins creating osteophytes or bone spurs. These spurs are not the disease itself but your body’s desperate attempt to widen the joint surface and stop instability.
Neuromuscular compensation compounds the problem. Your surrounding muscles including gluteus medius, piriformis, and iliopsoas are forced to contract permanently doing the job of failed ligaments. This leads to chronic muscle tightness, trigger points, and profound fatigue. Patients seek massage or stretching providing temporary relief, but because underlying instability remains, muscles tighten immediately again protecting the unstable joint.
Standard anti inflammatory approaches fail because they ignore this fundamental mechanical problem. NSAIDs like ibuprofen suppress inflammation but healing requires inflammation. The body’s natural repair process is an inflammatory cascade. By blocking this, NSAIDs actually inhibit collagen synthesis and ligament repair. Corticosteroids are even more problematic, being catabolic tissue breaking agents. They inhibit fibroblast activity, weaken collagen, and accelerate cartilage degeneration. Studies link repeated hip steroid injections to avascular necrosis where femoral head bone literally dies and collapses.
Prolotherapy offers physiological reversal of this degenerative cascade. Rather than suppressing your body’s response, prolotherapy stimulates it, triggering the proliferation or growth of new connective tissue to tighten loose ligaments.
Read next: Understanding the biomechanics of hip ligament function and failure at ARKA Anugraha Hospital.
How Prolotherapy Rebuilds Hip Ligament Strength

Prolotherapy succeeds for hip pain by targeting the root mechanical cause: ligament laxity. The treatment uses hyperosmolar dextrose, a naturally occurring sugar solution injected in high concentrations typically 12.5 to 25 percent. While simple, dextrose application in regenerative medicine triggers complex biological processes rebuilding connective tissue.
The osmotic gradient mechanism initiates repair. When hypertonic dextrose is injected at the fibro osseous junction where ligament attaches to bone, it creates a strong osmotic gradient causing temporary dehydration and cellular stress to local fibroblasts. This controlled shock does not kill cells but triggers them to release cytokines indicating tissue injury, essentially tricking your body into believing fresh injury occurred and waking up a stalled healing process.
The inflammatory cascade follows over days one through five. Released cytokines recruit your immune system to the site. Granulocytes and macrophages arrive cleaning debris and releasing growth factors including platelet derived growth factor, transforming growth factor beta, and connective tissue growth factor. During this phase, patients experience temporary stiffness or mild soreness, a clinical sign that healing cascade has been successfully initiated.
The proliferative phase spans weeks one through four. Stimulated by growth factors, fibroblasts migrate to the area and begin proliferating. They synthesize new extracellular matrix, primarily collagen. Initially Type III collagen, immature repair tissue, is deposited increasing the physical mass and thickness of your ligament. New capillaries form supplying oxygen and nutrients to repairing tissue, addressing the hypoxic low oxygen environment typical of chronic tendinopathy.
The remodeling phase extends months one through twelve and beyond. The new Type III collagen is remodeled into Type I collagen, which is denser, stronger, and more organized. Fibers align along lines of mechanical stress restoring your ligament’s tensile strength and elasticity. This tightening of the capsuloligamentous complex restores joint stability, eliminates abnormal shear forces, and allows your neuromuscular system to finally relax.
Beyond structural repair, prolotherapy has direct effects on pain pathways. High dextrose concentrations can block substance P, a pain neurotransmitter, from nociceptive nerve release. By stabilizing your joint, the constant aberrant firing of mechanoreceptors reduces, quieting your central nervous system’s alarm state.
Why Hip Steroid Injections Provide Temporary Relief But Accelerate Degeneration
Understanding corticosteroid injection limitations reveals why patients seeking lasting relief turn to regenerative alternatives. Hip steroid injections remain common practice for osteoarthritis, but their mechanism creates fundamental long term problems.
Corticosteroids powerfully suppress immune activity providing rapid initial pain relief. However, steroids are catabolic agents breaking down tissue. They turn off repair processes to stop pain signals. While inflammation reduces temporarily, the underlying ligament laxity and joint instability remain unaddressed. Your weakened ligaments cannot heal while steroid effects persist.
Recent radiological studies raise serious alarms regarding hip steroid injection complications. The hip joint appears uniquely vulnerable to adverse corticosteroid effects including avascular necrosis where steroids disrupt microcirculation to the femoral head causing bone cell death, subchondral insufficiency fractures from weakening bone structure beneath cartilage, and accelerated joint destruction with rapid osteoarthritis progression and femoral head collapse within months of injection.
The pattern is predictable. First steroid injection provides months of relief. Second gives weeks. Third may fail entirely because underlying structural damage worsens while symptoms are masked. Repeated steroids weaken spinal ligaments, thin bone density, and suppress immune function systemically.
Prolotherapy represents the opposite philosophy. Rather than suppressing while tissue degenerates, it stimulates genuine ligament repair and strengthening. Yes, improvement develops gradually over weeks to months rather than days. But results reflect permanent structural tissue formation that continues strengthening long after treatment ends. The collagen formed by prolotherapy is permanent, though maintenance of overall health prevents new damage.

The ARKA Integrative Hip Ligament Protocol
At ARKA Anugraha Hospital, prolotherapy is embedded within comprehensive care recognizing hip health reflects whole body health. Under Dr. Gaurang Ramesh’s functional medicine guidance, the approach addresses systemic factors that predispose patients to musculoskeletal failure.
The gut musculoskeletal axis represents a crucial connection. A compromised gut barrier called leaky gut allows bacterial toxins specifically lipopolysaccharides to translocate into bloodstream. These toxins trigger low grade systemic inflammatory response that degrades collagen and sensitizes hip joint pain receptors. Specific gut bacteria regulate regulatory T cell production. These immune cells are critical for tissue repair, migrating from gut to injury sites like your hip to coordinate the transition from inflammation to healing. Dysbiosis arrests this process, leaving your hip in chronic non healing inflammation.
Ligament repair is nutrient intensive requiring vitamin C for collagen cross linking, zinc and manganese for matrix synthesis, and amino acids proline and glycine for structural building blocks. Malabsorption from gut dysfunction essentially starves connective tissue rendering regenerative treatments less effective. At ARKA, patients undergoing prolotherapy receive gut health screening. Concurrent gut healing treatment lowers systemic inflammation and optimizes the biological terrain for tissue regeneration.
Hormonal influences profoundly affect ligament integrity. Estrogen has protective anabolic effects on collagen. The sharp estrogen decline during menopause strongly correlates with gluteal tendinopathy and hip osteoarthritis onset in women. Post menopausal women experience accelerated joint laxity from hormonal withdrawal. Chronic stress elevates cortisol levels. Cortisol is catabolic, breaking down protein and inhibiting fibroblast function. High stress literally impedes your body’s ability to knit ligaments back together.
Metabolic health links inextricably to joint health. In patients with insulin resistance or diabetes, excess blood sugar binds to collagen fibers forming advanced glycation end products. This glycation makes collagen brittle, less elastic, and resistant to normal remodeling. This sugaring of tendons makes them prone to tearing and slow to heal. Adipose tissue releases pro inflammatory cytokines called adipokines. Obesity is not just mechanical burden on your hip but biochemical assault.
Nutritional support provides raw materials for repair. Patients receive collagen boosting protocols including adequate protein intake, vitamin C crucial for collagen cross linking, zinc for enzymatic function, and hydration supporting the osmotic mechanism. Rehabilitation through progressive loading stimulates collagen alignment. Initial isometric exercises activate muscles without stressing joints. Remodeling phase introduces progressive loading aligning new collagen fibers along stress lines. Biomechanics re education on sitting, standing, and walking patterns prevents recurrence.
For patients like Meena whose story opened this article, ARKA’s integrative approach provided what conventional care could not: genuine ligament stabilization addressing the mechanical instability, metabolic dysfunction, and gut inflammation perpetuating degeneration rather than temporary symptom suppression awaiting inevitable surgery.
Your chronic hip pain does not have to mean accepting progressive limitation or facing joint replacement. When standard treatments fail to address ligament laxity and the systemic factors preventing healing, prolotherapy offers evidence based hope for preserving your native hip joint and restoring stable pain free function.

FREQUENTLY ASKED QUESTIONS
- What is ligament laxity and how does it cause chronic hip pain? Ligament laxity describes stretched, weakened ligaments that fail to properly stabilize your hip joint. Your hip’s three major ligaments including the iliofemoral, pubofemoral, and ischiofemoral ligaments normally provide static stability preventing excessive motion. When these ligaments stretch beyond their yield point through trauma or repetitive micro injury, collagen fibers fray and elongate creating looseness. This allows your femoral head to move excessively within the acetabulum creating micro instability. Instead of smooth gliding, your cartilage experiences shear grinding forces causing wear. Your muscles must contract permanently compensating for failed ligaments causing chronic deep aching, fatigue, and the sensation of your leg giving way. Prolotherapy specifically tightens these lax ligaments restoring proper joint mechanics.
- How does prolotherapy differ from cortisone injections for hip pain? Prolotherapy and cortisone represent opposite approaches. Cortisone is a catabolic steroid that suppresses immune activity providing rapid temporary relief but breaks down tissue over time. Steroids inhibit fibroblast activity, weaken collagen, and studies show accelerated cartilage degeneration with potential avascular necrosis where femoral head bone dies. Prolotherapy is anabolic, stimulating growth factors and collagen synthesis to rebuild ligament strength. While cortisone provides faster initial relief wearing off in weeks to months with diminishing returns, prolotherapy produces gradual improvement over months reflecting permanent structural tissue formation. The collagen built by prolotherapy is lasting, making it superior for long term hip stability versus repeated steroid injections that weaken the joint progressively.
- Why do my hip muscles stay tight even after massage and stretching? Your hip muscles remain chronically tight because they are compensating for underlying ligament laxity. When your primary stabilizers, the hip ligaments, fail to provide adequate joint stability, surrounding muscles including gluteus medius, piriformis, and iliopsoas are forced to contract permanently doing the ligaments’ job. This creates chronic muscle tightness, trigger points, and profound fatigue. Massage and stretching provide temporary relief by relaxing these overworked muscles, but they tighten immediately again because the fundamental instability forcing them to work overtime remains unresolved. Prolotherapy addresses the root cause by tightening loose ligaments. Once joint stability restores, your muscles no longer need to guard constantly and can finally relax permanently.
- Can prolotherapy help if my X-ray shows bone on bone hip arthritis? Yes, prolotherapy can provide significant relief even with advanced arthritis visible on X-rays. Pain in bone on bone hips often does not stem from the bone itself which has no nerve endings but from the capsule, ligaments, and synovium which are highly sensitive. When ligaments are lax, the unstable joint creates constant aberrant mechanoreceptor firing generating pain signals. By stabilizing the capsule and tightening ligaments, prolotherapy reduces this pathological signaling providing substantial pain relief and improved quality of life even if the X-ray appearance does not change. Additionally, stabilizing the joint reduces abnormal shear forces on remaining cartilage potentially slowing further degeneration. Many patients with severe radiological changes achieve meaningful functional improvement avoiding or postponing joint replacement surgery.
- How many prolotherapy sessions does chronic hip pain typically require? Most chronic hip conditions require three to six prolotherapy treatment sessions spaced four to six weeks apart. This interval allows the inflammatory cycle to complete and the proliferative phase to peak before next stimulation. Ligament repair is cumulative with each session building on previous collagen deposition. Severity influences treatment duration, with mild to moderate laxity often responding to three sessions while severe instability or advanced osteoarthritis may need six sessions. Clinical data indicates 80 to 90 percent of appropriately selected patients achieve significant relief defined as greater than 50 percent pain reduction and improved function. Unlike diminishing returns with steroids, prolotherapy results reflect permanent structural strengthening though overall health maintenance prevents new damage.
- Why does ARKA emphasize gut health when treating hip ligament problems? The gut musculoskeletal axis profoundly influences connective tissue healing. Compromised gut barriers called leaky gut allow bacterial endotoxins to enter bloodstream triggering systemic inflammation that degrades collagen and prevents proper ligament repair. Specific gut bacteria regulate regulatory T cells critical for tissue repair that migrate from gut to injury sites coordinating healing transitions. Dysbiosis arrests this process leaving hips in chronic non healing inflammation. Additionally, ligament repair requires intensive nutrients including vitamin C, zinc, manganese, and amino acids. Malabsorption from gut dysfunction starves connective tissue making regenerative treatments ineffective. At ARKA Anugraha Hospital under Dr. Gaurang Ramesh’s guidance, concurrent gut health treatment lowers systemic inflammation and optimizes biological terrain ensuring prolotherapy produces maximal results.
- What is the difference between prolotherapy and PRP or stem cells for hip pain? All are regenerative therapies but work differently. Prolotherapy using hypertonic dextrose is the foundational treatment acting as a signal recruiting your body’s existing repair cells to the injection site. It is highly effective and cost efficient for most hip ligament laxity cases. PRP platelet rich plasma involves concentrating your blood platelets to deliver higher doses of growth factors directly, useful for more severe degeneration. Stem cell therapy involves harvesting and injecting regenerative cells reserved for cases where the body’s response to dextrose is insufficient. At ARKA, treatment typically begins with dextrose prolotherapy due to its excellent efficacy and value. PRP or stem cells are considered for more severe degeneration or insufficient dextrose response, often used synergistically with prolotherapy.
- What lifestyle modifications are important during prolotherapy hip treatment? During the healing phase, avoid activities placing extreme tensile load on posterior hip capsule. This includes modifying deep squatting such as Indian toilet use, recommend commode chairs during recovery, and avoiding sitting cross legged on floors which stretches the very ligaments being tightened. These positions common in Indian lifestyles place maximal strain on healing structures. Critically, avoid NSAIDs like ibuprofen, diclofenac, or aspirin for at least one week before and two weeks after treatments as they block the healing inflammatory cascade prolotherapy initiates. Use acetaminophen for pain management instead. Gentle movement including walking encourages blood flow supporting repair, but avoid high impact activities or deep stretches during initial healing weeks. Progressive rehabilitation guided by physical therapy ensures proper biomechanics preventing recurrence.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
