
If you’ve been struggling with irregular periods, unexplained weight gain, or challenges with getting pregnant, you’ve likely encountered the terms “PCOS” and “PCOD.” They are often used interchangeably, creating a cloud of confusion for patients. Are they the same thing? Is one more serious than the other?
This confusion is more than just a matter of semantics. Understanding the critical distinction in the PCOS vs. PCOD debate is the single most important first step toward getting the right diagnosis, managing your symptoms, and creating an effective plan for your health and PCOS fertility goals.
As a leading center for integrative women’s health and fertility, we at ARKA Anugraha Hospital believe in empowering our patients with clarity. This article will break down everything you need to know about these two conditions, why the difference matters, and how a holistic approach can help you regain control of your health.
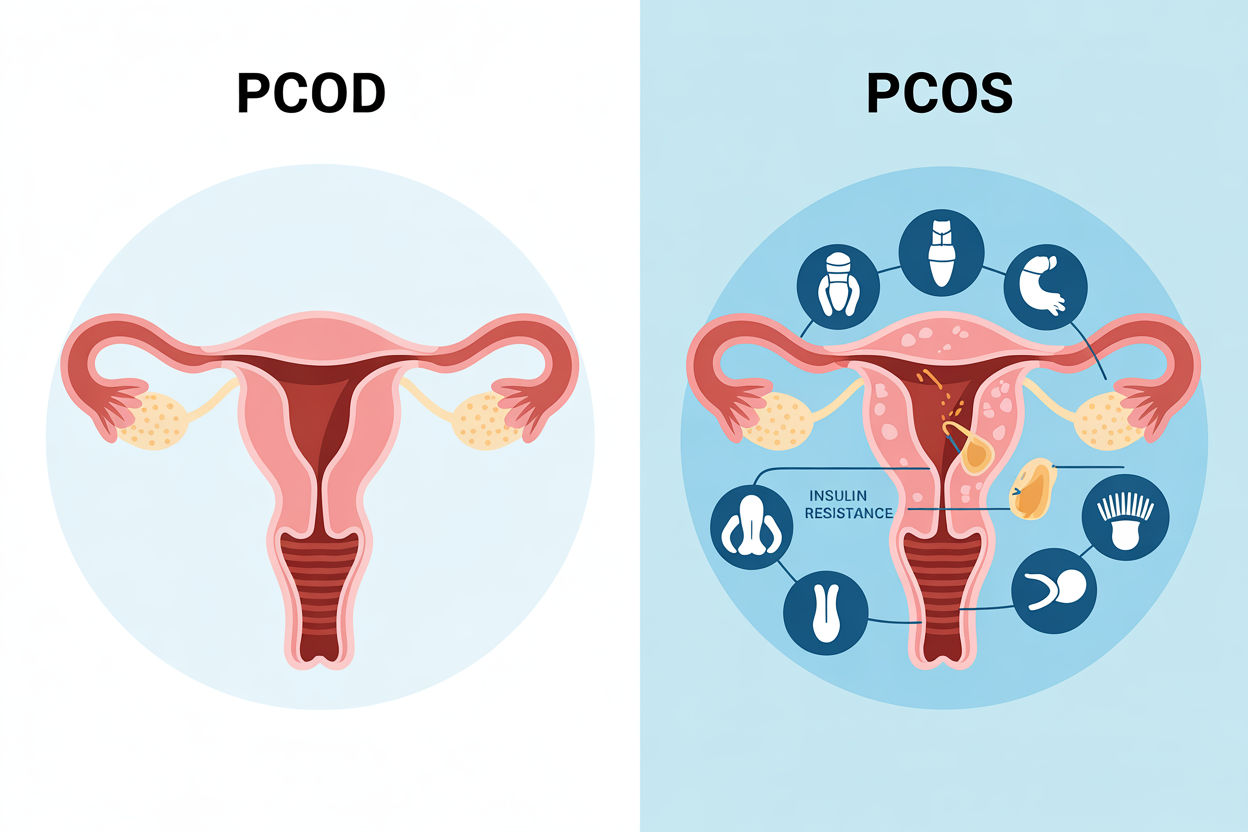
To understand the PCOS vs. PCOD difference, we must first define each term clearly. While they share some symptoms, they are not the same.
Think of Polycystic Ovarian Disease (PCOD) as a condition, not a syndrome. It is primarily a gynecological issue where the ovaries are not functioning perfectly.
This is where the distinction becomes critical. Polycystic Ovary Syndrome (PCOS) is not just a condition; it is a complex syndrome. A syndrome is a collection of symptoms that affect multiple systems in the body.
PCOS is a serious endocrine and metabolic disorder. It doesn’t just impact the ovaries; it affects your entire body, including how you process insulin and your overall hormonal balance.
To be diagnosed with PCOS, a patient doesn’t just need cysts on their ovaries. According to the internationally accepted Rotterdam Criteria, a diagnosis requires at least two of the following three features:
You can have PCOS without having “polycystic” ovaries, as long as you have irregular periods and high androgen levels. This is a key part of the PCOS vs. PCOD confusion.
This is the most common sign of PCOS. It can manifest as:
This is a direct sign that your body is not ovulating regularly, which is the primary reason PCOS impacts fertility.
Androgens are often called “male hormones,” but all women produce them in small amounts. In PCOS, the body produces an excess. This imbalance of androgen levels is responsible for many of the most distressing symptoms of PCOS:
A blood test can also confirm high levels of testosterone and other androgens, even if physical symptoms aren’t severe.
This is the ultrasound finding. It’s important to note that with modern, high-resolution ultrasound technology, many healthy, fertile women can have ovaries that look polycystic. This is why PCOM alone is not enough for a diagnosis. It must be combined with one of the other two criteria.

Now that we’ve defined them, let’s put them side-by-side. The PCOS vs. PCOD debate boils down to severity, cause, and whole-body impact.
This is the most significant difference and the key to understanding PCOS.
A majority of women with PCOS (up to 70-80%) have insulin resistance, regardless of their weight.
This creates a vicious cycle:
This metabolic dysfunction is the engine behind PCOS. PCOD, on the other hand, is not typically driven by significant insulin resistance.
Because PCOD is a milder condition, its long-term health risks are considered minimal if managed.
PCOS, however, is a lifelong condition that carries serious long-term health risks due to the underlying metabolic dysfunction:
Feature | PCOD (Polycystic Ovarian Disease) | PCOS (Polycystic Ovary Syndrome) |
Primary Issue | A condition of the ovaries. | A complex metabolic syndrome. |
Cause | Hormonal imbalance, often mild. | Driven by insulin resistance and high androgen levels. |
Prevalence | Very common (up to 33% of women). | Less common (6-13% of women). |
Ovulation | Often occurs, but irregularly. | Often absent (anovulation). |
Fertility | Can usually conceive with lifestyle changes or minor help. | A leading, but treatable, cause of infertility. |
Symptoms | Milder irregular periods, some weight gain. | Severe irregular periods, high androgen levels (acne, hirsutism), weight gain. |
Long-Term Risk | Low. | High risk of Type 2 Diabetes, heart disease, and endometrial cancer. |
This brings us to the most pressing question for many women: how does this affect my ability to get pregnant? The answer is “significantly.”
Pregnancy requires an egg. The core issue in PCOS fertility is anovulation—the lack of ovulation.
In a healthy PCOS patient, the hormonal chaos prevents a follicle from maturing and being released:
No egg means no chance for fertilization. This is why the first goal of any PCOS fertility plan is to restore ovulation.
This is a critical, often-overlooked point. For a long time, the focus was just on ovulation. We now know that the environment the eggs are growing in matters.
The high-insulin, high-androgen, and high-inflammation state of PCOS can be toxic to the developing eggs. This “oxidative stress” can damage the egg’s DNA and cellular machinery, leading to:
This is why simply forcing ovulation with medication isn’t always enough. A truly effective PCOS fertility plan must also address the underlying metabolic health to improve egg quality.
With PCOD, the picture is often brighter. Because the hormonal imbalance is milder and insulin resistance is not a primary driver, many women with PCOD still ovulate, just not on a perfect 28-day schedule. Their fertility challenge is often one of timing. Simple lifestyle changes or low-dose ovulation medication can be highly effective.

Understanding the PCOS vs. PCOD difference is vital because the treatment is not one-size-fits-all. A woman with mild PCOD does not need the same aggressive metabolic intervention as a woman with classic, insulin-resistant PCOS.
At ARKA Anugraha Hospital, we have built our reputation on providing the most comprehensive, integrative PCOS treatment in Bangalore. We don’t just treat the symptoms; we investigate and treat the root cause.
Our approach is a patient-centered, multi-step journey.
Your journey starts with clarity. We go beyond a simple ultrasound. Our PCOS treatment diagnostic panel in Bangalore includes:
This is the cornerstone of our PCOS treatment in Bangalore. We cannot medicate our way out of a metabolic problem.
For many with PCOS, lifestyle changes are supported with targeted medication:
When you are ready to conceive, our fertility specialists create a personalized plan.
As an integrative hospital, we bridge the gap between conventional medicine and holistic wellness. We often recommend a supportive regimen that may include:
Acupuncture: This ancient practice has been shown to help regulate hormone levels, reduce stress, and improve blood flow to the ovaries, supporting your fertility journey.

The PCOS vs. PCOD debate is more than just words. PCOD is a common condition of the ovaries. PCOS is a serious, lifelong metabolic syndrome.
Understanding this difference is the key to unlocking the right treatment. It dictates whether you need a simple lifestyle adjustment or a comprehensive, body-wide plan that addresses insulin resistance, high androgen levels, and chronic inflammation.
If you are struggling with irregular periods, fertility challenges, or other symptoms, you are not alone, and this is not your fault. A diagnosis is not an endpoint; it’s the starting point for a manageable, hopeful plan.
If you are looking for a team that understands these nuances and offers compassionate, expert PCOS treatment in Bangalore, we are here to help. Contact ARKA Anugraha Hospital today to schedule a consultation and take the first step from confusion to clarity.
A: This is a common and important question. While PCOD is a milder condition, if it’s left unmanaged and lifestyle factors like significant weight gain or poor diet worsen, it can trigger or unmask an underlying metabolic dysfunction like insulin resistance. This can cause the condition to progress and meet the full criteria for PCOS.
A: There isn’t one single cause. PCOS is understood to be a complex interplay of genetic and environmental factors. The main drivers include a genetic predisposition, chronic insulin resistance (which is often lifestyle-related), and low-grade inflammation, which all feed into the overproduction of androgen levels.
A: Yes, it is possible, though it can be more challenging. Because the primary issue in PCOS fertility is a lack of ovulation, some women with milder PCOS may ovulate occasionally and conceive. For many, significant lifestyle changes that improve insulin resistance (like weight loss and a low-glycemic diet) can be enough to restore regular ovulation and allow for natural conception.
A: It’s a direct chain reaction.
A: Our approach at ARKA Anugraha Hospital is truly integrative. We don’t just offer fertility drugs. We assemble a team including endocrinologists, gynecologists, fertility specialists, nutritionists, and holistic wellness experts to create a 360-degree plan. We focus on identifying and treating the root cause of your PCOS, whether it’s metabolic, hormonal, or inflammatory, to restore your long-term health, not just manage symptoms.
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore