Microbiome and Mood Connection: How Gut Bacteria Influence Mental Health

- Published on: 25/Dec/2025
- Posted By: Arka Health
The silent conversation shaping your mental health
For decades, mental health conditions such as anxiety, low mood, panic, and brain fog were viewed almost entirely as brain-based problems. Treatment focused on neurotransmitters, psychology, and emotional triggers. While these factors matter, modern medical research has revealed a deeper biological truth. The gut and the brain are in constant conversation, and this dialogue plays a major role in emotional regulation, stress resilience, and cognitive clarity.
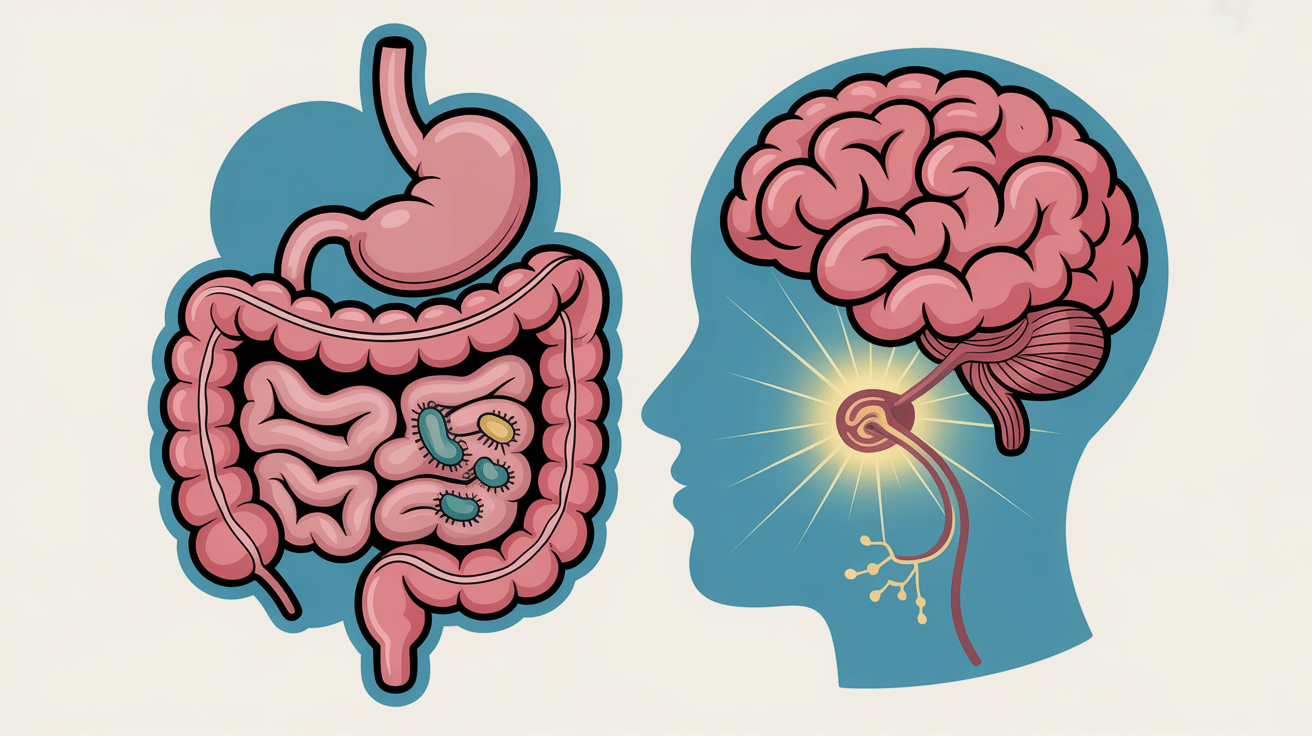
This communication system is known as the gut-brain axis. It links the digestive tract, the immune system, the nervous system, and the brain into a single integrated network. At the centre of this network is the gut microbiome, the trillions of bacteria living inside the intestines. These microorganisms are not passive passengers. They actively shape inflammation levels, neurotransmitter balance, hormone signalling, and even how the brain perceives stress.
Many people struggling with anxiety or depression also report digestive symptoms such as bloating, constipation, loose stools, food sensitivities, or discomfort after meals. These symptoms are often dismissed as unrelated or stress-induced. In reality, they may be early warning signs that the gut ecosystem is out of balance, quietly influencing mental health from below.
This article explains how gut bacteria influence mental health, why this connection is frequently missed, and how addressing gut health can become a powerful part of emotional recovery.
Understanding the gut as the second brain
The digestive system is far more complex than a tube for food processing. Embedded within the walls of the gastrointestinal tract is a dense network of neurons known as the enteric nervous system. This system contains hundreds of millions of nerve cells and can operate independently of the brain.
The enteric nervous system controls digestion, intestinal movement, enzyme release, and gut blood flow. It also senses pain, pressure, and inflammation within the gut. Because of its size and complexity, it is often referred to as the body’s second brain.
What makes this system particularly relevant to mental health is that it uses the same chemical messengers as the brain. Neurotransmitters such as serotonin, dopamine, GABA, and acetylcholine are active in the gut. In fact, the majority of the body’s serotonin is produced in the digestive tract, not the brain.
This shared chemistry explains why medications that act on brain neurotransmitters often cause digestive side effects. It also explains why gut dysfunction can directly affect mood, anxiety levels, and emotional stability.
The gut microbiome as a metabolic and signalling organ
The gut microbiome refers to the community of bacteria, viruses, and fungi that live inside the digestive tract. These microbes collectively contain far more genetic material than human DNA and provide metabolic functions that humans cannot perform alone.
Gut bacteria help break down dietary fibres, produce vitamins, regulate immune responses, and maintain the integrity of the intestinal lining. Beyond digestion, they act as chemical messengers, producing compounds that travel through the bloodstream and nervous system to influence brain function.
Because of this wide-ranging influence, the microbiome is now considered a functional organ rather than a passive collection of microbes. When balanced, it supports emotional resilience and mental clarity. When disrupted, it can become a driver of inflammation, neurotransmitter imbalance, and stress sensitivity.
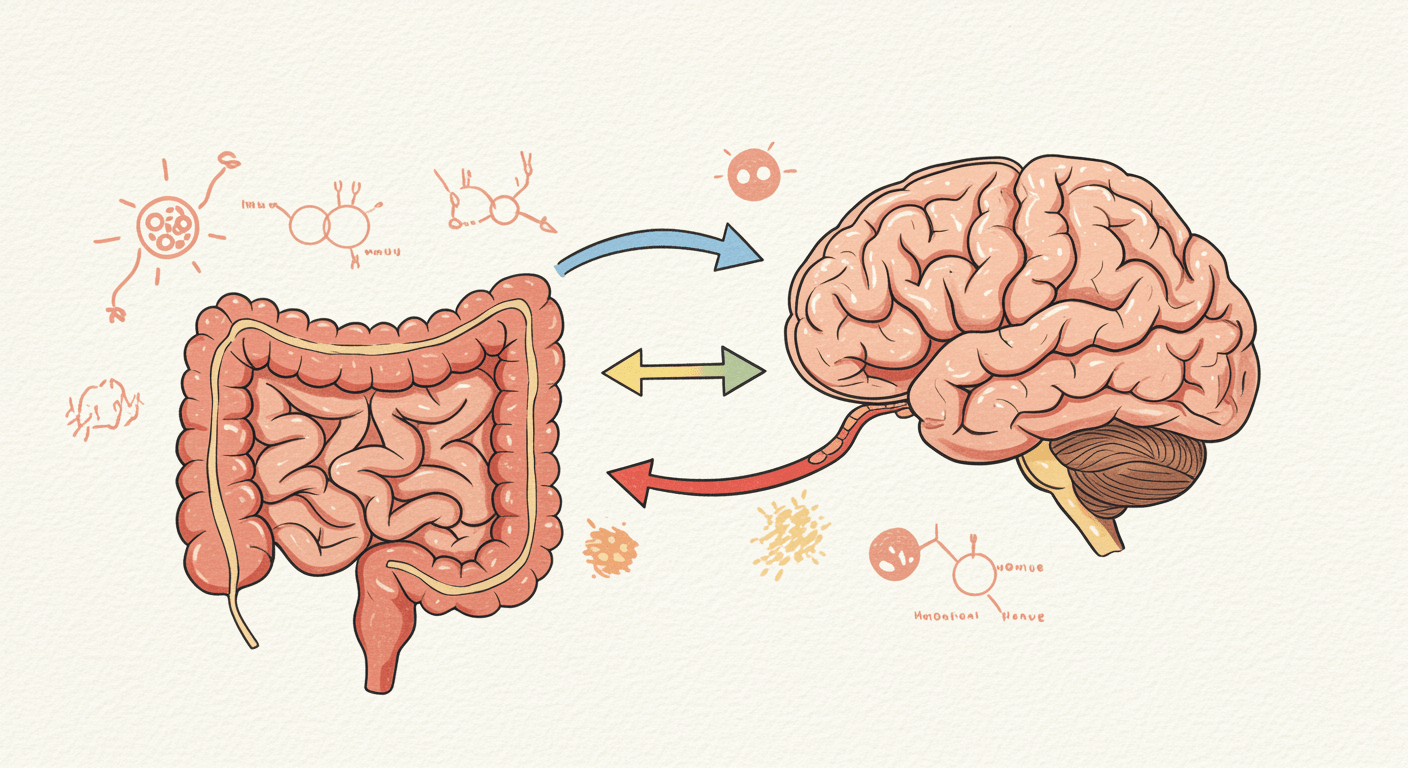
The gut-brain axis explained simply
The gut-brain axis is a two-way communication network connecting the gut and the brain. Signals constantly travel in both directions, allowing emotional states to influence digestion and gut health to influence mood.
This axis operates through three main pathways.
Nervous system signalling
The vagus nerve is the primary physical connection between the gut and the brain. It carries sensory information from the digestive tract upward to the brainstem and emotional centres of the brain. Interestingly, most of the signals travelling through this nerve go from the gut to the brain, not the other way around.
When the gut environment is inflamed or irritated, the vagus nerve transmits distress signals that the brain interprets as anxiety, unease, or low mood. A healthy gut sends calming signals that support emotional regulation.
Immune system signalling
A large proportion of the body’s immune cells reside in the gut. When the microbiome is imbalanced, harmful bacteria can trigger immune activation. This leads to the release of inflammatory molecules called cytokines.
These cytokines can cross into the brain or signal through the nervous system, altering mood, motivation, and cognitive function. Chronic low-grade inflammation is increasingly recognised as a contributor to depression and fatigue.
Chemical and hormonal signalling
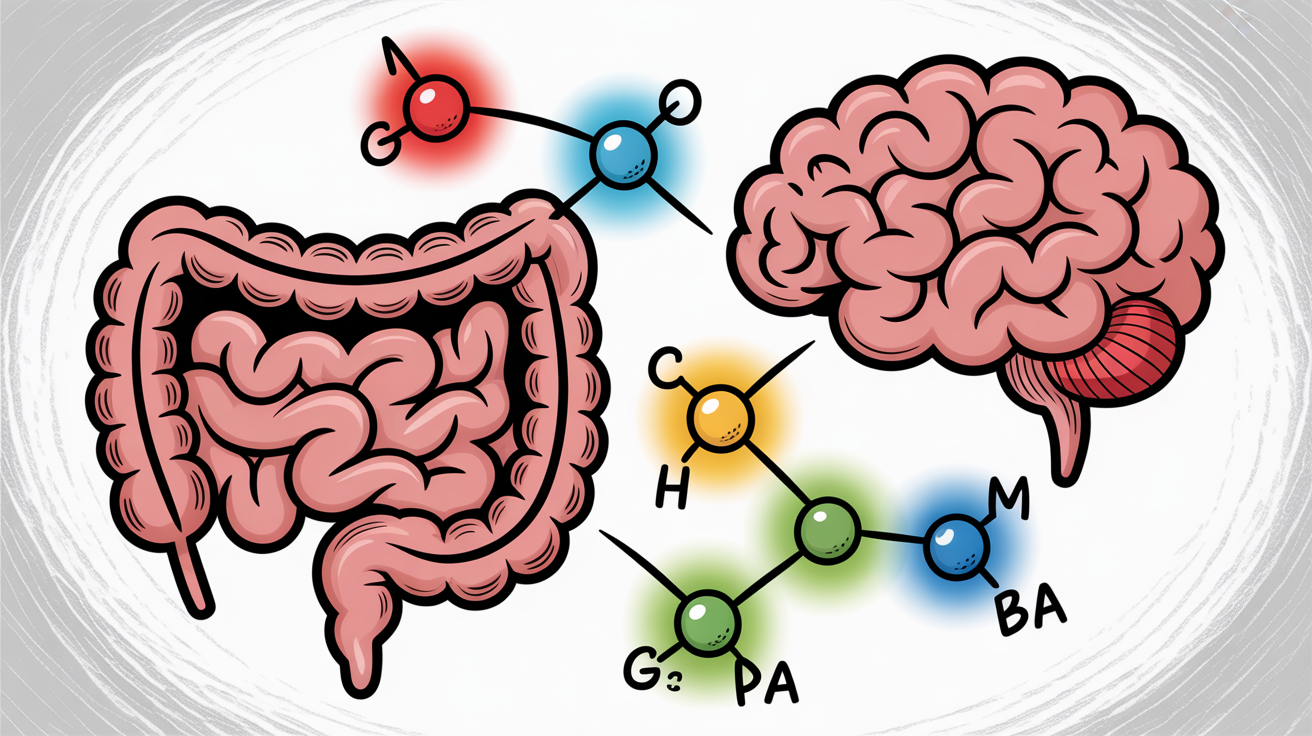
Gut bacteria produce neurotransmitters and metabolic by-products that influence brain chemistry. These include serotonin precursors, GABA, and short-chain fatty acids. Hormones involved in stress regulation are also influenced by gut activity.
Together, these pathways explain how changes in gut health can shape emotional experience, often without obvious digestive disease.
How gut bacteria influence neurotransmitters
One of the most important ways gut bacteria affect mental health is through neurotransmitter regulation.
Serotonin and mood stability
Serotonin plays a central role in mood balance, emotional wellbeing, and sleep regulation. While serotonin itself does not freely cross into the brain, the gut controls its production and the availability of its precursor, tryptophan.
When the gut is inflamed, tryptophan metabolism shifts toward inflammatory pathways, reducing the amount available for serotonin synthesis. This can contribute to low mood, irritability, and emotional volatility.
GABA and anxiety regulation
GABA is the brain’s primary calming neurotransmitter. Certain beneficial gut bacteria help produce GABA or influence its receptors through vagus nerve signalling.
When these bacterial populations are reduced, the nervous system becomes more reactive. This can manifest as anxiety, restlessness, poor sleep, or heightened stress responses.
Dopamine and motivation
Dopamine is involved in motivation, reward, and focus. Gut bacteria influence dopamine pathways indirectly through inflammation control and nutrient absorption. Poor gut health can reduce dopamine signalling, contributing to low motivation and mental fatigue.
Short-chain fatty acids and brain health
Short-chain fatty acids are produced when gut bacteria ferment dietary fibres. The most important of these is butyrate.
Butyrate serves as fuel for intestinal cells, helping maintain the gut barrier. It also reduces inflammation and influences gene expression in the brain. Adequate levels of butyrate support neuroplasticity, emotional regulation, and cognitive clarity.
Low levels of butyrate-producing bacteria are consistently observed in people with depression and chronic stress conditions. This highlights the importance of fibre intake and microbial diversity for mental wellbeing.
Gut permeability and inflammation driven mood changes
A healthy gut lining acts as a selective barrier, allowing nutrients to pass while keeping toxins out. When this barrier becomes compromised, a condition often referred to as increased intestinal permeability can develop.
In this state, bacterial fragments and toxins enter the bloodstream, triggering immune activation. The resulting inflammation can affect the brain, leading to symptoms such as fatigue, low mood, brain fog, and emotional numbness.
This process helps explain why many people experience both digestive discomfort and psychological symptoms without clear findings on routine medical tests.
Anxiety, depression, and the microbiome connection
People with anxiety disorders often show reduced microbial diversity and higher levels of inflammatory bacteria. Their stress response systems tend to be overactive, producing higher cortisol levels in response to everyday challenges.
Gut imbalance amplifies this response by impairing vagus nerve signalling and increasing inflammation. This creates a feedback loop where stress worsens gut health and gut dysfunction heightens anxiety.
Depression is increasingly understood as an inflammatory condition in many individuals. Elevated inflammatory markers and immune activation are common findings.
Gut dysbiosis contributes to this inflammation by disrupting immune balance and neurotransmitter pathways. This explains why some people do not respond well to conventional antidepressants alone.
Brain fog is a common complaint among individuals with gut issues. Toxins produced by certain bacteria, along with inflammatory mediators, can impair concentration, memory, and mental clarity.
These symptoms often worsen after meals or during digestive flares, further supporting the gut-brain link.
Why this connection is often missed
Despite growing evidence, the gut-mental health connection is frequently overlooked in clinical practice.
Modern healthcare is highly specialised. Digestive symptoms are treated separately from psychological symptoms, even when they coexist. Standard investigations focus on structural disease rather than functional imbalance.
As a result, many people are told their tests are normal while their symptoms persist. Without addressing gut health, treatment may remain incomplete.
How gut imbalance shows up in real life
Many people do not experience gut-brain dysfunction as a dramatic illness. Instead, it shows up subtly and progressively.
A professional may notice increasing anxiety during workdays, paired with bloating after lunch and poor sleep at night. Another person may struggle with low mood that worsens after meals, frequent sugar cravings, or unexplained fatigue despite normal blood tests. Some experience panic attacks after food poisoning, antibiotics, or prolonged stress, followed by months of digestive sensitivity.
These patterns are often treated as separate problems. In reality, they are frequently connected by microbiome imbalance, inflammation, and disrupted gut-brain signalling.
Dysbiosis and its mental health impact
Dysbiosis refers to an imbalance in gut bacteria where beneficial microbes are reduced and harmful or opportunistic species dominate.
Common contributors include repeated antibiotic use, chronic stress, irregular eating patterns, processed foods, poor sleep, and untreated digestive infections. Over time, dysbiosis alters immune signalling, neurotransmitter production, and stress hormone regulation.
Symptoms of dysbiosis may include bloating, gas, constipation, loose stools, food intolerance, brain fog, anxiety, irritability, and low mood. The longer this imbalance persists, the more entrenched the mental health symptoms can become.
Why conventional testing often misses the problem
Most routine medical investigations are designed to detect structural disease. Endoscopy, colonoscopy, and standard blood panels look for ulcers, tumours, severe inflammation, or infection.
Functional gut issues do not always show up on these tests. A person can have normal scans and still experience significant gut-brain dysfunction.
This gap leads many patients to feel dismissed or told that symptoms are stress-related without deeper physiological evaluation. Addressing function rather than structure is where integrative and functional medicine becomes valuable.
How the condition is evaluated clinically

A gut-focused mental health evaluation begins with a detailed clinical history.
Key areas explored include digestive symptoms, antibiotic exposure, stress patterns, sleep quality, dietary habits, food reactions, and the timing of mental health symptoms relative to meals or infections.
Based on this assessment, targeted investigations may be considered.
This test evaluates microbial diversity, beneficial and harmful bacteria, digestive enzyme output, inflammatory markers, and gut barrier health. It provides insight into dysbiosis patterns that influence mood and cognition.
Small intestinal bacterial overgrowth can contribute to anxiety, bloating, and brain fog through fermentation gases and toxin production. Breath testing helps identify hydrogen or methane overgrowth patterns.
Deficiencies in B12, magnesium, iron, zinc, and omega-3 fats can worsen anxiety and depression. Gut dysfunction often impairs absorption of these nutrients.
Delayed food reactions can drive low-grade inflammation that affects both the gut and the brain. Identifying these triggers helps reduce immune activation.
Treatment principles for gut-driven mental health symptoms
Treating gut bacteria and mental health requires a layered, root-cause approach rather than symptom suppression alone.
The goal is to reduce inflammation, restore microbial balance, support neurotransmitter production, and stabilise nervous system signalling.
Removing aggravating factors
This includes addressing infections, bacterial overgrowth, inflammatory foods, excessive sugar, alcohol, and unnecessary medications that irritate the gut lining.
Stress reduction is not optional. Chronic stress directly alters gut permeability and microbial balance.
Supporting digestion and absorption
Poor digestion leads to fermentation, bloating, and nutrient deficiency. Supporting stomach acid, digestive enzymes, and bile flow can significantly improve symptoms.
Rebuilding the microbiome
Probiotics are most effective when chosen strategically. Certain strains influence anxiety and mood more than others. Random supplementation is often ineffective.
Prebiotic fibres are introduced carefully to nourish beneficial bacteria without worsening symptoms.
Repairing the gut lining
Nutrients such as L-glutamine, zinc carnosine, omega-3 fats, and soothing plant compounds support gut barrier repair. This reduces inflammatory signalling to the brain.
Nervous system regulation
Breathing practices, sleep optimisation, and gentle movement help restore vagal tone and calm the stress response. Without this step, gut healing remains incomplete.
The Indian diet and gut-brain health
Traditional Indian diets offer powerful tools for microbiome balance when used appropriately.
Fermented foods such as curd and buttermilk support beneficial bacteria. Fibre-rich vegetables, legumes prepared correctly, and cooled rice provide prebiotic substrates.
Spices like turmeric, cumin, fennel, and ginger reduce inflammation and support digestion. Ghee provides butyrate, a key short-chain fatty acid for gut and brain health.
Equally important is what to limit. Excess refined flour, sugar, late-night meals, and ultra-processed foods disrupt microbial balance and worsen mental health symptoms.
Consistency matters more than perfection. Small, sustainable changes create long-term improvement.
One integrated approach at ARKA Anugraha Hospital
At ARKA Anugraha Hospital, gut and mental health are evaluated as part of a connected physiological system rather than isolated symptoms.
The approach focuses on identifying the biological drivers behind anxiety, depression, brain fog, and emotional instability. Functional diagnostics, clinical correlation, and personalised treatment protocols are used to address dysbiosis, inflammation, nutrient deficiencies, and stress physiology.
Dr Gaurang Ramesh brings a combined perspective of gastroenterology and functional medicine, allowing both structural safety and functional depth. Treatment plans are designed to restore gut health while supporting mental resilience, without overpromising or replacing necessary psychiatric care.
This integrative model is particularly helpful for individuals with persistent symptoms, treatment-resistant anxiety or depression, or overlapping digestive complaints.
The path forward
Mental health is not confined to the brain. It is shaped by the gut, the immune system, the nervous system, and daily lifestyle patterns.
When gut bacteria fall out of balance, the effects can quietly influence mood, anxiety, energy, and cognition. Addressing this connection does not replace psychological support or medication when needed. Instead, it strengthens the biological foundation on which mental health depends.
For many people, healing begins not by changing their thoughts, but by restoring the environment within their gut.
Frequently Asked Questions
Can gut bacteria really affect anxiety and depression?
Yes. Gut bacteria influence inflammation, neurotransmitter balance, stress hormones, and vagus nerve signalling, all of which affect mood and anxiety.
Is gut-related depression different from other depression?
The symptoms may feel similar, but gut-related depression often involves inflammation, digestive symptoms, food sensitivity, and poor response to medication alone.
How do I know if my mental health issues are gut-related?
Clues include digestive symptoms, worsening mood after meals, history of antibiotics or food poisoning, brain fog, and fatigue.
Can probiotics improve mental health?
Certain strains may help, but probiotics work best when chosen based on symptoms and gut status rather than taken randomly.
What is the gut-brain axis in simple terms?
It is the two-way communication system between your gut and your brain that influences digestion, mood, stress, and immunity.
Does stress damage gut bacteria?
Yes. Chronic stress alters gut permeability, reduces beneficial bacteria, and increases inflammation.
Can diet alone fix gut-related anxiety?
Diet is foundational, but most people also need targeted support for digestion, microbiome balance, and stress regulation.
How long does gut healing take?
Improvements may begin within weeks, but deeper restoration often takes two to three months or longer.
Is SIBO linked to anxiety and brain fog?
Yes. Bacterial overgrowth can produce gases and toxins that affect cognition and mood.
Are Indian fermented foods enough for probiotics?
They are helpful but may not provide consistent therapeutic strains needed for specific conditions.
Does leaky gut cause mental health symptoms?
Increased gut permeability can drive inflammation that affects brain function and mood regulation.
Should mental health treatment always include gut evaluation?
Not always, but it is especially important when digestive symptoms, inflammation, or treatment resistance are present.
Can children and young adults have gut-related anxiety?
Yes. Diet, antibiotics, stress, and infections can affect gut-brain health at any age.
Is this approach safe alongside psychiatric treatment?
Yes. Gut-focused care is supportive and can complement conventional mental health treatment.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
