Low AMH, Not Low Hope: Paths to Pregnancy for ARKA Anugraha Hospital

Published on: 26/Nov/2025
Posted By: Arka Health

Executive Summary: Redefining the Narrative of Diminished Ovarian Reserve
The diagnosis of Diminished Ovarian Reserve (DOR), clinically quantified by low levels of Anti-Müllerian Hormone (AMH), represents one of the most challenging and emotionally turbulent junctures in reproductive medicine. For decades, this biomarker has been wielded as a definitive gavel, often prematurely sentencing couples to the conclusion that biological parenthood is beyond reach. However, the evolving landscape of assisted reproductive technology (ART), when harmonized with functional and integrative medicine, tells a radically different story. Low AMH is a measure of quantity, not quality; it is a clinical signal indicating the need for strategic urgency and tailored intervention, rather than an absolute barrier to conception.
This comprehensive research report, commissioned for ARKA Anugraha Hospital in Bangalore, serves as a definitive clinical and holistic guide. It is designed to deconstruct the monolithic label of “Low AMH” into actionable, scientifically grounded pathways. We move beyond the simplistic interpretation of blood values to explore the sophisticated interplay of ovarian physiology, mitochondrial bioenergetics, the gut-gonad microbiome axis, and advanced stimulation protocols like DuoStim and Estrogen Priming.
Central to this report is the unique value proposition of ARKA Anugraha Hospital. Situated in the heart of JP Nagar, with deep connections to Singaporean technological standards and a philosophy rooted in holistic healing, ARKA stands at the vanguard of a new fertility paradigm. By integrating the surgical precision of experts like Dr. Saraswathi Ramesh and Dr. Ramesh Makam with the functional medicine insights of Dr. Gaurang Ramesh, the institution offers a “whole-person” approach that is rare in the fragmented landscape of modern healthcare. This document details how ARKA’s multidisciplinary framework—encompassing advanced embryology, regenerative PRP therapies, and metabolic optimization—transforms the prognosis for patients navigating the complexities of low ovarian reserve.
Chapter 1: The Biological Paradigm of Ovarian Reserve
%20in%20one%20cycle,%20depicting%20sequential%20waves%20of%20follicle%20growth..png)
1.1 The Physiology of Anti-Müllerian Hormone (AMH)
To understand the clinical approach to low AMH, one must first master the underlying physiology. Anti-Müllerian Hormone is a dimeric glycoprotein belonging to the transforming growth factor-beta (TGF-β) superfamily. In the adult female, it is produced exclusively by the granulosa cells of pre-antral and small antral follicles in the ovary. These are the follicles that have been recruited from the primordial resting pool but have not yet entered the selection phase for ovulation.
The clinical utility of AMH stems from its relative stability. Unlike Follicle-Stimulating Hormone (FSH), which fluctuates dramatically based on the feedback loops of the menstrual cycle, AMH levels remain reasonably constant throughout the cycle, offering a reliable snapshot of the “functional” ovarian reserve. It serves as a proxy for the size of the primordial follicle pool. However, a critical distinction must be maintained: AMH is a marker of follicular quantity, not oocyte competence. A lower AMH level correlates with a reduced yield of oocytes during controlled ovarian hyperstimulation (COH), but it does not inherently predict the chromosomal constitution (ploidy) or the fertilization potential of the eggs that are retrieved. This distinction is the bedrock of hope for patients with low AMH; as long as viable oocytes exist, the potential for a healthy embryo remains, provided the retrieval and culture conditions are optimized.
1.2 Interpreting the Numbers: A Spectrum, Not a Binary
The stratification of AMH levels is essential for setting realistic patient expectations and designing appropriate treatment protocols. The reference ranges typically utilized in clinical practice are:
- Robust/Normal Reserve: > 1.0 ng/mL
- Low Reserve: 0.5 – 1.0 ng/mL
- Very Low / Diminished Ovarian Reserve (DOR): < 0.5 ng/mL
- Ultralow Reserve: < 0.1 ng/mL 3
It is crucial to interpret these values in the context of chronological age. A 30-year-old woman with an AMH of 0.5 ng/mL faces a fundamentally different prognosis than a 42-year-old woman with the same level. The younger patient, despite having fewer eggs, typically maintains a higher rate of euploidy (chromosomal normality). Conversely, the older patient faces the “double hit” of reduced quantity and age-related decline in oocyte quality. Research indicates that women with very low AMH (<0.5 ng/mL) can still achieve reasonable pregnancy rates, particularly if they are under 35, because the “gold” is still present, even if it is harder to mine.
1.3 The Myth of the “Biological Cliff”
Popular culture often depicts fertility as falling off a cliff. In reality, ovarian aging is a continuum. The attrition of the follicular pool accelerates after age 37, a phenomenon termed “atresia.” However, the ovaries do not simply shut down overnight. Even in states of severe DOR, the ovaries often continue to recruit follicles, albeit in smaller cohorts. The clinical challenge is that standard IVF protocols, designed for “average” responders, often fail to rescue these small cohorts, leading to cycle cancellations. The approach at ARKA Anugraha is to reject the one-size-fits-all methodology in favor of individualized protocols that respect the unique biological tempo of the low-reserve ovary.
Chapter 2: Diagnostic Precision at ARKA Anugraha
2.1 The Singapore Connection: World-Class Standards
In the crowded fertility market of Bangalore and Mysore, ARKA Anugraha distinguishes itself through its adherence to international standards, specifically leveraging technology and expertise rooted in Singapore’s advanced medical ecosystem. The fertility center boasts 25+ years of international experience, bringing rigorous quality control to its embryology laboratories. In IVF, the lab is the “womb” for the first few days of life. Air purity, temperature stability, and culture media quality are paramount. The adoption of Singaporean protocols ensures that even the few fragile eggs retrieved from a low AMH patient are given the optimal environment to survive and thrive.
2.2 Comprehensive Diagnostic Profiling
Diagnosis at ARKA goes beyond a simple blood test. The team, led by Dr. Saraswathi Ramesh and Dr. Ramesh Makam, employs a multi-modal diagnostic strategy to build a complete picture of reproductive potential.
2.2.1 Antral Follicle Count (AFC) and Ultrasound
While AMH is biochemical, the Antral Follicle Count (AFC) is anatomical. Performed via high-resolution transvaginal ultrasound, the AFC counts the number of resting follicles (2-10mm) visible at the start of the cycle. A discordance between AMH and AFC (e.g., low AMH but decent AFC) can sometimes indicate issues like Vitamin D deficiency or laboratory error, rather than true ovarian depletion. The ultrasound also assesses ovarian blood flow (Doppler studies), crucial for determining if the ovaries are receiving adequate vascular support to respond to medication.
2.2.2 The Hormonal Triad: FSH, LH, and Estradiol
Basal FSH levels are a classic marker of reserve; as the ovary struggles, the pituitary creates more FSH to whip it into action. However, FSH levels can be deceptive. If a patient has a functional cyst producing estrogen, or if the “Estrobolome” in the gut is recirculating estrogen (a specialty interest of Dr. Gaurang Ramesh), the FSH may be artificially suppressed into the “normal” range. ARKA’s protocol involves testing FSH, Luteinizing Hormone (LH), and Estradiol (E2) simultaneously to unmask these silent physiological compensations.
2.2.3 Advanced Immunological and Metabolic Screening
Recognizing that the ovaries do not exist in a vacuum, the diagnostic workup often includes screening for autoimmune thyroiditis (TPO antibodies), insulin resistance (HOMA-IR), and markers of systemic inflammation (CRP). Conditions like Hashimoto’s thyroiditis or undiagnosed pre-diabetes can severely impair egg quality, rendering even a “good” number of eggs non-viable. This holistic diagnostic lens is a direct reflection of the hospital’s integrative philosophy.
Chapter 3: The Science of Stimulation – Protocols for the "Poor Responder"
The standard “Long Protocol” or high-dose antagonist protocol often fails the low AMH patient. Flooding a low-reserve ovary with massive doses of gonadotropins can lead to receptor downregulation or “fry” the few available eggs. ARKA Anugraha utilizes a nuanced range of stimulation strategies designed to coax, rather than force, the ovaries.
3.1 The DuoStim Protocol: A Game Changer
For patients with severe DOR or those racing against the biological clock (e.g., age > 40), time is the most precious resource. The DuoStim (Double Stimulation) protocol represents a paradigm shift in IVF efficiency.
- Mechanism: Traditionally, IVF cycles utilize only the follicular phase (first half) of the menstrual cycle to recruit eggs. However, ovarian folliculogenesis occurs in waves. The DuoStim protocol capitalizes on this by initiating a second round of stimulation immediately after the first egg retrieval, during the luteal phase.
- Efficacy Data: Research indicates that the second “luteal” wave often yields a higher number of oocytes than the first. Studies have shown that DuoStim can increase the rate of obtaining at least one euploid (genetically normal) blastocyst from 42.3% to 65.5% compared to a single stimulation. Furthermore, it condenses two months of treatment into one, significantly reducing the “Time to Live Birth” and minimizing the dropout rate caused by patient fatigue.
- Clinical Application: At ARKA, this protocol is particularly favored for patients who need to accumulate embryos for Pre-implantation Genetic Testing (PGT) before attempting a transfer.
3.2 Estrogen Priming Protocols
One of the hallmarks of low ovarian reserve is “asynchronous” follicular growth—a “lead follicle” grows rapidly, suppressing the others, resulting in the retrieval of only one mature egg despite the presence of several smaller ones.
- The Strategy: Estrogen Priming involves administering estradiol (oral or patch) in the luteal phase of the cycle preceding the stimulation. This suppresses the premature rise of FSH, preventing the early selection of a dominant follicle. When stimulation begins, the cohort of follicles is synchronized, allowing them to grow together and resulting in the retrieval of a larger group of mature eggs.
- Impact: This method helps to “quiet” the ovaries and reset the receptors, often improving the response to gonadotropins in the subsequent cycle.
3.3 Minimal Stimulation (Mini-IVF) and Natural Cycle
For patients with extremely low AMH (e.g., < 0.1 ng/mL), the ovaries may simply lack the receptor density to respond to high-dose medication. In these cases, “more is not better.”
- Mini-IVF: This approach uses low doses of oral medications like Clomiphene Citrate or Letrozole, supplemented with small doses of injectables. The goal is quality over quantity—aiming for 2-3 high-quality eggs rather than trying (and failing) to get 10.
- Natural Cycle IVF: This involves tracking the single dominant follicle selected by the body naturally and retrieving it. It avoids the side effects and costs of heavy medication. While the yield is low (one egg), the implantation rates per embryo can be surprisingly high because the uterine lining has not been subjected to supraphysiological hormone levels.
3.4 Growth Hormone (GH) Adjuvants
To further enhance mitochondrial function within the oocyte, ARKA Anugraha may employ Growth Hormone (GH) as an adjuvant during stimulation. GH receptors are present on granulosa cells and oocytes. Supplementation has been shown to upregulate the synthesis of Insulin-like Growth Factor 1 (IGF-1), which works synergistically with FSH to promote follicle growth. Meta-analyses suggest that GH co-treatment can improve clinical pregnancy rates and live birth rates in poor responders by improving oocyte competence.
Chapter 4: The Laboratory – Technological Excellence

The journey from oocyte to embryo is perilous. At ARKA Anugraha, the embryology lab serves as a sanctuary, equipped with technology designed to mitigate the vulnerabilities of low-quality eggs.
4.1 Intracytoplasmic Morphologically Selected Sperm Injection (IMSI)
While ICSI (injecting a sperm into an egg) is standard, IMSI takes it a step further. Using high-magnification microscopy (6000x vs. the standard 400x), embryologists can examine the sperm head for vacuoles or structural defects that might be missed otherwise. For couples where male factor infertility compounds low AMH, IMSI ensures that the precious few eggs are fertilized only by the most structurally perfect sperm, thereby maximizing fertilization rates.
4.2 Time-Lapse Embryo Culture
Traditional embryo culture requires removing embryos from the incubator to check them under a microscope, exposing them to fluctuations in temperature and pH. Time-lapse technology (such as the EmbryoScope) involves built-in cameras that take photos of the developing embryos every few minutes.
- Benefits: This allows for continuous monitoring without disturbing the culture environment. Furthermore, artificial intelligence (AI) algorithms analyze the cleavage patterns to predict which embryos have the highest implantation potential. For a low AMH patient with only two embryos, knowing which one to transfer first is critical.
4.3 Laser Assisted Hatching (LAH)
Embryos from older women or those with poor oocyte quality often have a thickened outer shell (zona pellucida), which can impair hatching and implantation. Laser Assisted Hatching involves using a precision laser to thin or create a small breach in the zona, facilitating the embryo’s escape and attachment to the uterine lining. This technique is routinely available at ARKA to boost implantation rates in difficult cases.
Chapter 5: The Integrative Approach – The Gut-Gonad Axis
Perhaps the most distinctive feature of ARKA Anugraha is its embrace of the “Gut-Gonad Axis,” a frontier of medicine championed by Dr. Gaurang Ramesh. While traditional IVF centers focus solely on the reproductive organs, ARKA recognizes that the ovaries are deeply influenced by the body’s metabolic and microbial environment.9
5.1 The Microbiome and Fertility
Emerging research has established a bidirectional communication channel between the gut microbiota and the reproductive system.
- The Estrobolome: This refers to a specific collection of bacteria in the gut capable of metabolizing estrogens. These bacteria produce beta-glucuronidase, an enzyme that deconjugates estrogen, allowing it to be reabsorbed into the bloodstream. Dysbiosis (an imbalance of gut bacteria) can disrupt this process. Too much activity leads to estrogen dominance (associated with endometriosis and cysts); too little leads to estrogen deficiency (impairing follicular growth).
- Oxidative Stress and Inflammation: A “leaky gut” allows endotoxins (LPS) to enter the circulation, triggering systemic inflammation. This chronic inflammatory state can damage the vascular supply to the ovaries and increase oxidative stress within the follicular fluid, directly harming the DNA of developing eggs.23
5.2 Therapeutic Interventions for the Gut
Dr. Gaurang Ramesh’s protocols often involve a “pre-conception detox” or gut restoration program.
- Probiotics and Prebiotics: Targeted supplementation to restore healthy flora, specifically focusing on strains that support the estrobolome.
- Dietary Modification: Elimination of inflammatory foods (processed sugars, trans fats) that feed pathogenic bacteria.
Impact: Animal studies have shown that germ-free mice (lacking a microbiome) have a significantly shorter reproductive lifespan and fewer eggs. By restoring the microbiome, ARKA aims to extend the functional window of the ovaries and improve the quality of the eggs remaining.
Chapter 6: Nutritional & Metabolic Optimization

Fueling the machinery of reproduction requires more than just calories; it requires specific substrates for mitochondrial energy and hormonal synthesis.
6.1 The Mediterranean Diet: Evidence-Based Nutrition
The Mediterranean Diet is widely regarded as the gold standard for fertility nutrition. Characterized by a high intake of vegetables, legumes, nuts, fruits, and olive oil, and a moderate intake of fish and poultry, this diet is rich in antioxidants and anti-inflammatory compounds.
- Clinical Evidence: Studies have shown that high adherence to the Mediterranean Diet is associated with a higher number of available embryos and improved clinical pregnancy rates in IVF. The diet’s high content of monounsaturated fats and low glycemic index helps regulate insulin sensitivity, which is crucial for ovarian function.
- Implementation: At ARKA, nutritional counseling helps patients integrate these principles, ensuring they are “eating for egg quality” months before the first injection.
6.2 Targeted Supplementation Strategy
While no pill can generate new eggs, specific supplements can enhance the bioenergetics of the existing pool.
- Coenzyme Q10 (CoQ10): The oocyte contains more mitochondria than any other cell. As eggs age, their mitochondria become inefficient at producing ATP, the energy currency required for chromosomal segregation. CoQ10 (specifically Ubiquinol) acts as a mitochondrial fuel. Clinical trials demonstrate that CoQ10 supplementation improves ovarian response and egg quality.
- Dehydroepiandrosterone (DHEA): DHEA is an androgen precursor. Androgens are essential for the early stages of follicle development (pre-antral to antral transition). Supplementation with DHEA for 6-12 weeks prior to IVF has been shown to increase the pool of recruitable follicles and reduce aneuploidy rates.
- Antioxidants: Supplements like Melatonin, Vitamin E, and N-Acetyl Cysteine (NAC) are used to combat oxidative stress in the follicular fluid.
Chapter 7: Regenerative Medicine – Ovarian Rejuvenation
For patients who have exhausted standard options, ARKA Anugraha offers cutting-edge regenerative therapies.
7.1 Intra-Ovarian Platelet-Rich Plasma (PRP)
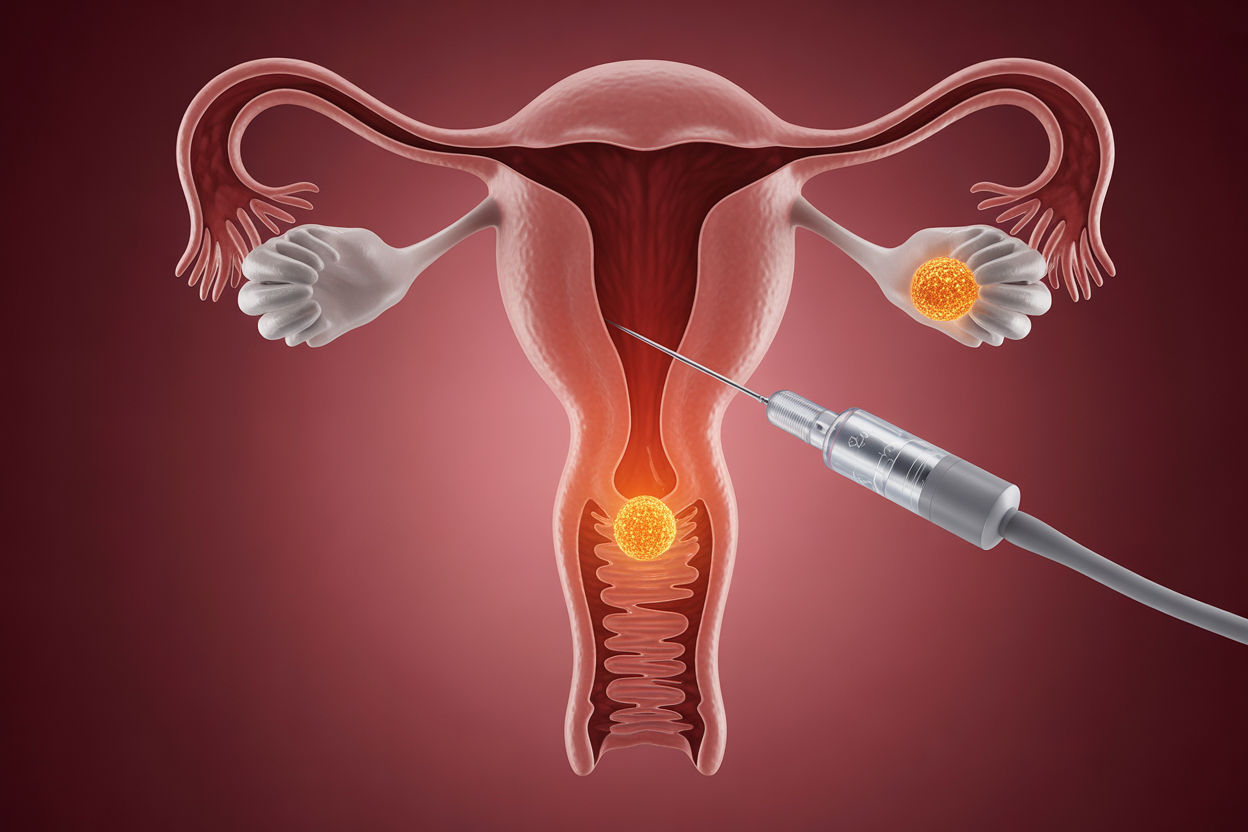
PRP therapy involves injecting a concentration of the patient’s own platelets directly into the ovaries.
- The Science: Platelets are reservoirs of growth factors (PDGF, VEGF, TGF-β, EGF) that promote angiogenesis (blood vessel growth) and tissue regeneration. The theory is that these factors can “wake up” dormant primordial follicles that are otherwise unresponsive to hormones.
- Outcomes: A meta-analysis of 10 trials showed that PRP treatment resulted in a significant increase in AMH levels and Antral Follicle Count (AFC). It has also been linked to the resumption of menses in perimenopausal women and improved pregnancy rates in women with Poor Ovarian Response (POR). At ARKA, this procedure is performed under ultrasound guidance or laparoscopy, often as a prelude to an IVF cycle.
7.2 Stem Cell Therapy Context
While PRP is the current clinical standard, research into Ovarian Stem Cells (OSCs) is ongoing. The regenerative potential of PRP is thought to be partly mediated by its interaction with these resident stem cells, creating a microenvironment conducive to follicular rescue.
Chapter 8: Lifestyle Medicine – Yoga, Acupuncture, and Stress
The physiological impact of stress on fertility is mediated through the Hypothalamic-Pituitary-Adrenal (HPA) axis. Chronic stress elevates cortisol, which can suppress the pulsatile release of GnRH, leading to anovulation or luteal phase defects.
8.1 Fertility Yoga
Yoga is a therapeutic modality integrated into the care at ARKA Anugraha. Specific asanas are prescribed to enhance pelvic blood flow and reduce sympathetic nervous system overdrive.
- Key Poses: Supta Baddha Konasana (Reclining Bound Angle) opens the pelvic girdle; Viparita Karani (Legs Up the Wall) promotes venous return and relaxation. These practices not only aid physical perfusion of the ovaries but also offer a psychological anchor for patients during the stressful IVF process.
8.2 Acupuncture
Acupuncture is widely used to support IVF outcomes.
- Mechanism: It is believed to modulate the release of neurotransmitters and hormones, improve uterine blood flow (thickening the endometrium), and reduce uterine contractility (preventing expulsion of the embryo).
- Protocol: A typical protocol might involve weekly sessions for 8-12 weeks prior to retrieval to improve ovarian response, followed by sessions immediately before and after embryo transfer.
Chapter 9: Financial Planning & Logistics
9.1 Cost of Treatment in Bangalore
Navigating the financial aspect of IVF is critical. Bangalore offers competitive pricing compared to global standards.
- Standard IVF Cycle: ₹1,50,000 – ₹2,50,000. This typically includes stimulation, retrieval, and transfer.
- IVF with ICSI: ₹1,70,000 – ₹3,00,000.
- Additional Costs: Medications (variable based on dosage), Embryo Freezing (~₹20,000 – ₹40,000 per year), and specialized tests like PGT-A (~₹20,000 per embryo).
- DuoStim Cost: Since it involves two stimulations and two retrievals, the cost is higher, but often packaged to be less than two separate cycles.
9.2 ARKA Anugraha’s Accessibility
Located in JP Nagar, ARKA Anugraha offers a range of room options from General Wards (₹2,500/night) to Deluxe Suites (₹10,000/night), catering to diverse economic backgrounds. The hospital partners with major insurance providers (Bajaj Allianz, HDFC Ergo, etc.) for covered procedures (though standard IVF is often excluded from basic health insurance, ancillary procedures like hysteroscopy may be covered). The transparency in pricing is a core tenet of their patient-centric approach.
Chapter 10: Patient Narratives & Conclusion
10.1 Stories of Hope
The clinical data is reinforced by human stories. Patients like Shannon (AMH 0.23) and Tanya (AMH 0.01) demonstrate that even with ultralow numbers, persistence and the right protocol (often involving DHEA and customized stimulation) can lead to motherhood.4 These narratives underscore the importance of looking beyond the “label” of Low AMH.
10.2 Conclusion: A Sanctuary for the Future
ARKA Anugraha Hospital represents a convergence of hope and science. By refusing to view Low AMH as a final verdict, the team—comprising Dr. Saraswathi, Dr. Makam, Dr. Gaurang, and their support staff—opens doors that were previously thought closed. Through the synergy of Singaporean technology, regenerative medicine (PRP), holistic gut health restoration, and precision stimulation (DuoStim), they offer a path to pregnancy that is as compassionate as it is effective.
Low AMH is a diagnosis, not a destiny. With the comprehensive care model at ARKA Anugraha, the journey to parenthood is supported by the full weight of modern science and ancient healing wisdom.
Frequently Asked Questions (FAQ)
Q1: Does Low AMH mean I have no eggs left?
A: No. It means the quantity is reduced, but you still have eggs. Women with low AMH can and do conceive, both naturally and with assistance.
Q2: How does ARKA Anugraha’s “Gut-Gonad” approach help fertility?
A: By treating gut dysbiosis and inflammation, we improve hormonal balance (estrogen metabolism) and reduce systemic oxidative stress, which can improve the quality of the eggs you have left.
Q3: What is the advantage of the DuoStim protocol?
A: DuoStim allows us to collect two batches of eggs in one menstrual cycle (one from the follicular phase, one from the luteal phase), doubling the opportunity to find a healthy embryo in a shorter timeframe.
Q4: Is PRP painful?
A: Intra-ovarian PRP is a minimally invasive procedure performed under sedation or anesthesia. Discomfort is minimal and typically resolves quickly.
Q5: Can I improve my egg quality with diet?
A: Yes. Following an anti-inflammatory diet like the Mediterranean Diet, rich in antioxidants and healthy fats, has been scientifically proven to improve IVF outcomes.
Q6: Where is the hospital located?
A: ARKA Anugraha Hospital is at #2, 15th Cross, 6th Phase, J.P. Nagar, Bengaluru, Karnataka 560078.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
