IVF Add-Ons Demystified: ICSI, PGT-A, PRP, ERA

Published on: 27/Nov/2025
Posted By: Arka Health

1. Executive Summary: The Evolving Landscape of Assisted Reproduction in India
The field of reproductive medicine has undergone a seismic shift over the last decade, transitioning from a discipline focused primarily on the mechanical facilitation of fertilization to a complex, multi-disciplinary ecosystem of genetic screening, endometrial receptivity analysis, and regenerative therapies. For patients in Mysuru and the broader Karnataka region, navigating this landscape is increasingly challenging. The rise of “IVF add-ons”—supplementary procedures offered alongside standard In Vitro Fertilization (IVF)—has introduced a new layer of decision-making that is as financially significant as it is medically complex.
This report serves as an exhaustive clinical and operational analysis of these technologies, specifically tailored for the patient demographic and clinical philosophy of ARKA Anugraha Hospital. Unlike traditional fertility clinics that may view these add-ons solely through a technological lens, ARKA Anugraha’s approach, led by experts such as Dr. Gaurang Ramesh, integrates advanced surgical interventions with functional medicine. This integrative model acknowledges that while technologies like Intracytoplasmic Sperm Injection (ICSI) or Preimplantation Genetic Testing for Aneuploidy (PGT-A) address specific mechanical or genetic failure points, the underlying “soil”—the patient’s metabolic, immune, and microbiome health—remains the critical determinant of success.
In the following sections, we provide a granular analysis of the four primary add-ons—ICSI, PGT-A, PRP, and ERA—alongside minor adjuvants like Embryo Glue and Assisted Hatching. We scrutinize the global evidence base, referencing data from the Human Fertilisation and Embryology Authority (HFEA), the European Society of Human Reproduction and Embryology (ESHRE), and Indian clinical contexts. Furthermore, we explore the distinct economic landscape of fertility treatments in Mysuru and Bangalore, providing a transparent cost-benefit analysis that empowers patients to distinguish between essential medical interventions and experimental adjuncts.
2. The Biological Imperative: Standard IVF vs. ICSI
2.1 The Mechanism of Fertilization
To understand the necessity and efficacy of Intracytoplasmic Sperm Injection (ICSI), one must first appreciate the complexity of physiological fertilization and standard IVF. In a natural conception or standard IVF setting, fertilization is a selection event. Thousands of spermatozoa surround the oocyte (egg). These sperm must undergo capacitation, a biochemical maturation process that destabilizes the acrosome (the sperm’s head cap) and creates a hyper-activated motility pattern. The sperm must then penetrate the cumulus oophorus (a cloud of cells surrounding the egg), bind to the zona pellucida (the egg’s outer shell), and undergo the acrosome reaction to release enzymes that digest a path through the shell.
Standard IVF mimics this natural selection in a laboratory dish. It relies on the sperm’s inherent ability to recognize, bind to, and penetrate the egg. This method allows for natural selection barriers to filter out functionally incompetent sperm. However, when sperm parameters are compromised—specifically in cases of severe oligospermia (low count), asthenospermia (poor motility), or teratospermia (poor morphology)—this natural barrier becomes an insurmountable wall.
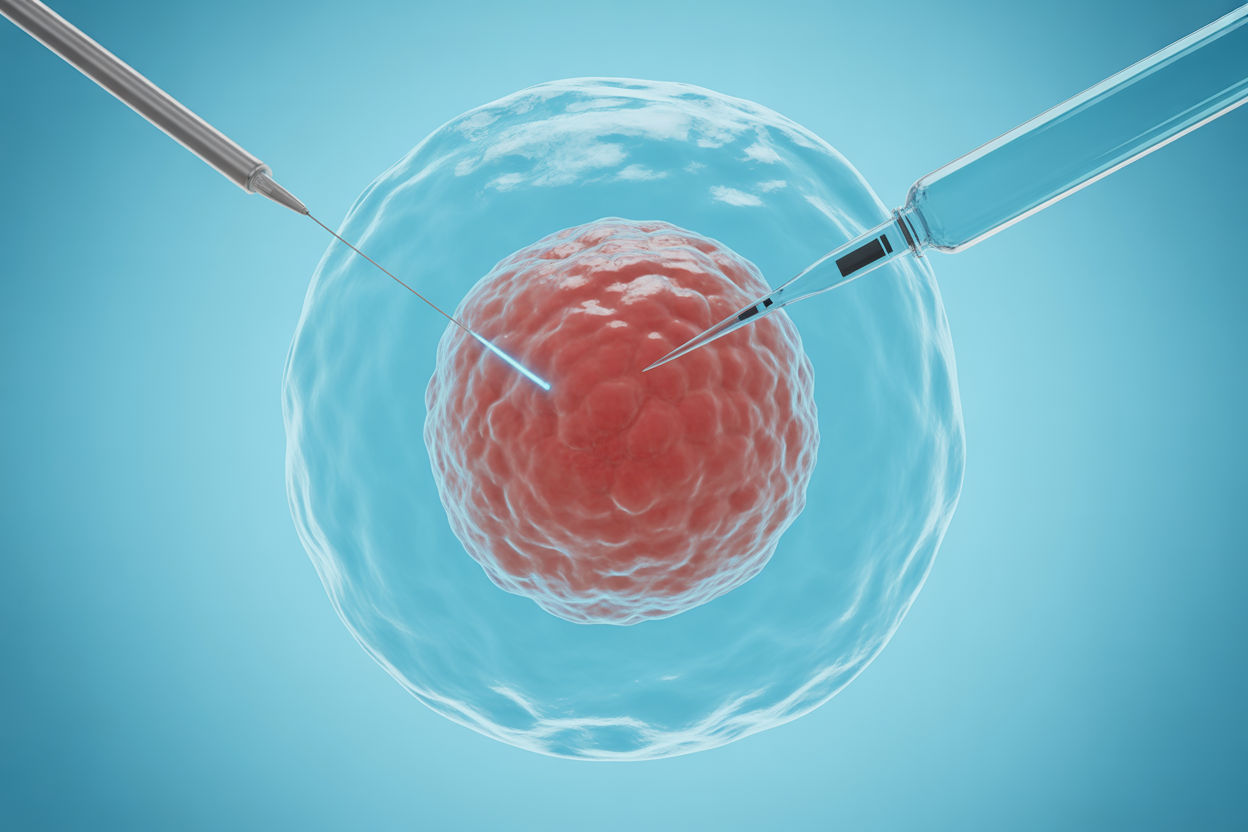
2.2 Intracytoplasmic Sperm Injection (ICSI): A Micromanipulation Revolution
ICSI, introduced in the early 1990s, bypasses these natural barriers entirely. It is a micromanipulation technique where a single sperm is selected by an embryologist, immobilized to break its tail membrane (releasing necessary activation factors), and injected directly into the ooplasm (cytoplasm) of the egg.
This technique revolutionized the treatment of male factor infertility. It enabled men with virtually zero motility or extremely low sperm counts—including those requiring surgical sperm retrieval (TESA/PESA)—to father biological children. The procedure effectively renders the zona pellucida irrelevant as a barrier to fertilization.
2.3 ICSI vs. IVF: Evidence-Based Indications and Contraindications
A critical debate in modern reproductive medicine is the routine use of ICSI for non-male factor infertility. Many clinics globally and in India have shifted toward 100% ICSI utilization, operating under the assumption that bypassing natural barriers will inevitably yield higher fertilization rates. However, the data does not support this indiscriminate application.
2.3.1 Male Factor Infertility
The evidence is unequivocal: for couples with severe male factor infertility, ICSI is the gold standard. It significantly improves fertilization rates and live birth outcomes compared to standard IVF, which would likely result in total fertilization failure in these cases.
2.3.2 Non-Male Factor Infertility
For couples with tubal factor infertility, ovulation disorders, or unexplained infertility where sperm parameters are normal, the superiority of ICSI is highly contested. Large-scale studies and meta-analyses indicate that ICSI offers no significant advantage in live birth rates (LBR) for non-male factor cases.
- Fertilization Rates: While ICSI ensures sperm entry, standard IVF often yields higher fertilization rates per retrieved oocyte in non-male factor cases because the oocytes are not subjected to the mechanical stress of injection.
- Embryo Quality: Some studies suggest that bypassing natural selection via ICSI might result in embryos with lower developmental potential if the selected sperm carried subtle defects that natural selection would have filtered out.
- Cycle Cancellation: Research indicates that patients undergoing IVF for unexplained infertility actually have lower cancellation rates compared to those using ICSI, challenging the notion that ICSI is a “safety net” against failure.
2.3.3 Specific Indications for ICSI beyond Male Factor
Despite the lack of benefit for general non-male factor cases, specific scenarios mandate ICSI usage:
- Preimplantation Genetic Testing (PGT-A): If a couple is opting for genetic testing, ICSI is strongly recommended to avoid “genetic contamination.” In standard IVF, multiple sperm adhere to the zona pellucida. Their DNA can inadvertently be included in the trophectoderm biopsy, leading to erroneous results. ICSI ensures only one sperm’s DNA is present.
- Cryopreserved Oocytes: The process of vitrification (freezing) can cause hardening of the zona pellucida, making natural fertilization difficult. Therefore, ICSI is standard for fertilized frozen eggs.
- Previous Fertilization Failure: For couples who have experienced total fertilization failure in a previous standard IVF cycle, ICSI is the indicated rescue procedure.
2.4 Cost Implications in Mysuru and Bangalore
The financial distinction between ICSI and standard IVF is relevant for patients at ARKA Anugraha.
- Standard IVF Cost: Generally ranges between ₹95,000 to ₹1,50,000 per cycle in the region.
- ICSI Cost: The additional micromanipulation expertise and equipment typically add ₹25,000 to ₹40,000 to the base cost. Patients should be wary of “package” deals that default to ICSI without a medical indication, as this increases costs without a proven increase in success rates for non-male factor etiologies.
3. Genomic Precision: Preimplantation Genetic Testing (PGT-A)
3.1 The Genetic Basis of Implantation Failure
One of the most profound realizations in reproductive biology is the high prevalence of chromosomal errors in human embryos. An embryo requires 46 chromosomes (23 pairs) to be genetically normal, or euploid. An embryo with missing or extra chromosomes is termed aneuploid. Aneuploidy is the single most common cause of implantation failure and early miscarriage.
The rate of aneuploidy is strictly correlated with maternal age.
- Under 35: Approximately 30-40% of blastocysts are aneuploid.
- Age 40: Approximately 60-70% of blastocysts are aneuploid.
- Age 42+: Over 85% of blastocysts are aneuploid.16
3.2 The PGT-A Workflow
Preimplantation Genetic Testing for Aneuploidy (PGT-A) allows embryologists to screen embryos before transfer. The process involves:
- Biopsy: On Day 5 or 6 of development (blastocyst stage), 5-10 cells are removed from the trophectoderm (the layer destined to become the placenta). The inner cell mass (fetus) remains untouched.
- Cryopreservation: The embryo must be frozen while the cells are sent to a specialized genetics laboratory for Next-Generation Sequencing (NGS).
- Analysis: The DNA is analyzed to count chromosomes. Results categorize embryos as Euploid (Normal), Aneuploid (Abnormal), or Mosaic (Mixed).
3.3 Efficacy and the “Add-On” Debate
The utility of PGT-A is a subject of intense global debate. The HFEA in the UK currently rates PGT-A as “Red,” indicating no robust evidence for routine use to improve live birth rates per cycle started.2 However, this rating contrasts with clinical practices in the US and many private Indian clinics where it is widely utilized.
3.3.1 Arguments for PGT-A
- Reduced Miscarriage Rates: By avoiding the transfer of aneuploid embryos, PGT-A significantly lowers the clinical miscarriage rate.
- Reduced Time to Pregnancy: Patients avoid the time lost in transferring embryos that are destined to fail. For a 40-year-old woman with 5 blastocysts, only 1 might be normal. Without PGT-A, she might undergo 4 failed transfers (taking 6-8 months) before finding the viable one. PGT-A identifies the viable one immediately.
- Single Embryo Transfer (SET): PGT-A empowers clinics to confidently transfer a single embryo, virtually eliminating the risk of multiple pregnancies (twins/triplets) which carry high obstetric risks.
3.3.2 Arguments Against PGT-A
- Invasiveness: The biopsy procedure involves laser dissection and removal of cells. While robust blastocysts tolerate this well, there is a theoretical risk of damaging the embryo, particularly if the biopsy technique is suboptimal.
- Mosaicism: The phenomenon of mosaicism—where an embryo has both normal and abnormal cells—complicates decision-making. High-resolution NGS platforms now detect low-level mosaicism. Historically, these embryos were discarded. Recent data suggests mosaic embryos can self-correct and result in healthy live births. PGT-A may therefore lead to the discarding of potentially viable embryos.
- No Improvement in Cumulative LBR: For younger women (<35), studies show PGT-A does not increase the cumulative live birth rate per retrieval. It merely selects the embryo faster.
3.4 PGT-A in India: Regulatory and Economic Context
In India, the Pre-Conception and Pre-Natal Diagnostic Techniques (PCPNDT) Act strictly prohibits sex selection. PGT-A reports in India are rigorously redacted to exclude sex chromosomes (XX/XY), reporting only on the autosomes (chromosomes 1-22) and the presence of aneuploidy.
Cost Analysis:
PGT-A is a significant financial undertaking in India.
- Biopsy and Testing Fee: Typically ₹20,000 to ₹30,000 per embryo.
- Total Cycle Cost: A patient with 4 blastocysts could see their IVF bill increase by ₹1,00,000 to ₹1,20,000 solely for testing, plus the mandatory cost of Frozen Embryo Transfer (FET).
At ARKA Anugraha, the recommendation for PGT-A is likely personalized. It is most medically justifiable for women over 37, couples with a history of Recurrent Pregnancy Loss (RPL), or those with known chromosomal translocations (using PGT-SR).
4. Regenerative Medicine: Platelet-Rich Plasma (PRP)
4.1 The Science of Autologous Healing
Platelet-Rich Plasma (PRP) represents the intersection of regenerative medicine and fertility. The therapy utilizes the patient’s own blood, which is centrifuged to concentrate platelets to 3-5 times physiological levels. These platelets are rich in alpha-granules containing growth factors such as Platelet-Derived Growth Factor (PDGF), Vascular Endothelial Growth Factor (VEGF), and Transforming Growth Factor (TGF-beta).
4.2 PRP for Thin Endometrium
A receptive endometrium is crucial for implantation, with a thickness of >7mm generally considered optimal. For patients with persistent thin lining (refractory thin endometrium) who do not respond to exogenous estrogens, PRP is an emerging therapy.
- Procedure: PRP is infused into the uterine cavity via a catheter, similar to an IUI procedure, typically 48-72 hours before progesterone administration.
- Mechanism: The growth factors are hypothesized to stimulate angiogenesis (new blood vessel formation) and cell proliferation in the endometrial basal layer.
- Evidence: Several small-scale studies and meta-analyses suggest PRP can improve endometrial thickness and clinical pregnancy rates in this specific subgroup of patients.22 Given the autologous nature of the product (using the patient’s own blood), the safety profile is high, with minimal risk of immune reaction or infection.
4.3 PRP for Ovarian Rejuvenation
A more controversial application is intra-ovarian PRP for women with Diminished Ovarian Reserve (DOR) or Premature Ovarian Insufficiency (POI).
- Procedure: Under sedation and ultrasound guidance (similar to egg retrieval), PRP is injected directly into the ovarian cortex.
- Mechanism: The theory posits that growth factors can activate dormant primordial follicles or even ovarian stem cells, termed “reawakening” the ovary.
- Clinical Outcomes: While some clinics report “miraculous” resumption of menstruation or spontaneous pregnancies in menopausal women 24, robust randomized controlled trials are lacking. The data indicates that while PRP may transiently increase Anti-Müllerian Hormone (AMH) levels and antral follicle counts (AFC), it does not reliably reverse ovarian aging.
- Success Rates: Studies report spontaneous pregnancy rates of roughly 4-5% and IVF pregnancy rates of ~12-17% in these poor-prognosis cohorts following PRP.
Cost: In the Mysuru/Bangalore region, ovarian PRP is priced between ₹25,000 to ₹50,000 per session, making it a significant “add-on” consideration.
5. Timing is Everything: Endometrial Receptivity Analysis (ERA)
5.1 The Window of Implantation (WOI)
Successful implantation requires synchronization between a viable embryo and a receptive endometrium. This period of receptivity is known as the Window of Implantation (WOI). Standard protocols assume this window opens roughly 120 hours (5 days) after the start of progesterone (P+5).
However, genomic research suggests that up to 25-30% of patients with Repeated Implantation Failure (RIF) may have a displaced WOI.
- Pre-receptive: The lining needs more time (e.g., transfer on P+6 or P+7).
- Post-receptive: The lining has already passed its peak (e.g., transfer on P+4).
5.2 The ERA Test: Transcriptomics in Action
The ERA test is a molecular diagnostic tool that analyzes the expression of 248 genes involved in endometrial receptivity.
- Process: The patient undergoes a “mock” cycle with hormones exactly as they would for a transfer. Instead of an embryo transfer, an endometrial biopsy is taken on the theoretical day of transfer.
- Results: The sample is sequenced to determine the transcriptomic signature. The result classifies the endometrium as Receptive or Non-Receptive, providing a specific recommendation for the timing of progesterone exposure for the subsequent real transfer.
5.3 Controversy and Current Status
While initially hailed as a breakthrough, recent large-scale studies (such as the IGENOMIX-backed randomized trial) have tempered enthusiasm. Data indicates that for good prognosis patients (first-time IVF), routine ERA testing does not improve live birth rates.27 Its utility is now largely confined to the RIF population—patients who have failed to conceive after the transfer of 3 or more euploid embryos.
Cost: The ERA test is expensive, ranging from ₹35,000 to ₹50,000 in India, excluding the cost of the mock cycle medications.
6. Minor Adjuvants: Embryo Glue and Assisted Hatching
6.1 Embryo Glue: Adhesion, Not Magic
“Embryo Glue” is a colloquial term for a culture medium enriched with Hyaluronan, a macromolecule naturally found in the uterine fluid.
- Mechanism: Hyaluronan increases the viscosity of the transfer medium and interacts with CD44 receptors on the embryo and endometrium, potentially facilitating the initial apposition and adhesion phases of implantation.
- Evidence: A Cochrane review suggests a modest increase in clinical pregnancy rates (from ~33% to ~40%).
- Cost: Relatively low, typically adding ₹5,000 to ₹15,000 to a cycle.37 Given the low risk and potential benefit, it is often a standard offering in premium packages.
6.2 Assisted Hatching
Assisted Hatching (AH) involves using a laser to thin or breach the zona pellucida of the embryo on Day 3 or Day 5.
- Mechanism: It helps the blastocyst “hatch” from its shell, a prerequisite for implantation.
- Indications: Recommended for older women (whose zona may be thicker/harder), frozen-thawed embryos (hardening due to vitrification), or embryos with naturally thick zonae.
- Cost: ₹10,000 to ₹20,000 per cycle.
7. The ARKA Advantage: Integrative and Functional Medicine

While the add-ons described above focus on the technological manipulation of the embryo or endometrium, ARKA Anugraha Hospital distinguishes itself through an Integrative and Functional Medicine approach, championed by Dr. Gaurang Ramesh.3 This philosophy posits that fertility is not an isolated variable but a systemic output of overall health.
7.1 The Gut-Fertility Axis
A core tenet of the functional approach at ARKA is the connection between the gut microbiome and reproductive health.
- The Estrobolome: Specific bacteria in the gut possess the gene for beta-glucuronidase, an enzyme that regulates estrogen metabolism. Dysbiosis (imbalance) in the gut can lead to impaired estrogen excretion, causing reabsorption of estrogen into the bloodstream. This “Estrogen Dominance” is a key driver of conditions like Endometriosis, Fibroids, and Polycystic Ovary Syndrome (PCOS), all of which impair fertility.
- Systemic Inflammation: “Leaky Gut” (intestinal permeability) allows endotoxins (LPS) to enter the circulation, triggering chronic low-grade inflammation. This systemic inflammation can impair oocyte quality, disrupt the Hypothalamic-Pituitary-Ovarian (HPO) axis, and create a hostile uterine environment for implantation.
7.2 The 5R Protocol in Fertility
Dr. Gaurang Ramesh employs functional medicine protocols such as the “5R” approach to optimize patients before they undergo expensive IVF procedures 42:
- Remove: Eliminate inflammatory foods (gluten, dairy, processed sugar), toxins, and low-grade infections (parasites, yeast).
- Replace: Add digestive enzymes and stomach acid (Betaine HCL) to ensure nutrients crucial for egg quality (Zinc, B12, Iron) are actually absorbed.
- Reinoculate: Introduce beneficial bacteria (Lactobacillus, Bifidobacterium) via high-quality probiotics and prebiotics to restore the estrobolome.
- Repair: Use nutrients like L-Glutamine, Omega-3s, and Aloe Vera to heal the gut lining and reduce systemic inflammation.
- Rebalance: Address lifestyle factors—stress management (cortisol regulation), sleep hygiene, and emotional well-being.
7.3 Why This Matters for “Add-Ons”
This integrative preparation acts as a biological force multiplier.
- ICSI: Works better if the sperm DNA fragmentation (often caused by oxidative stress and poor diet) is reduced through lifestyle changes.
- Implantation: An anti-inflammatory diet can potentially reduce the need for aggressive immunological add-ons by calming the immune system naturally.
- Success Rates: By optimizing the “soil” (the mother’s body), the expensive “seed” (the IVF embryo) has the highest chance of thriving.
8. Economic Analysis: IVF Costs in Mysuru and Bangalore (2024-2025)
For patients planning treatment at ARKA Anugraha or similar centers in Karnataka, transparent cost estimation is vital. The following table aggregates data from current market rates in the region.
Procedure / Add-On | Estimated Cost Range (INR) | Notes on Necessity |
Standard IVF Cycle | ₹1,20,000 – ₹1,80,000 | Base cost (Consults, scans, retrieval, lab). Meds (~₹50k-₹80k) often extra. |
ICSI Add-on | ₹25,000 – ₹40,000 | Essential for male factor; optional for others. |
PGT-A (Genetics) | ₹20,000 – ₹30,000 per embryo | High cost; recommended for age >37 or recurrent loss. |
ERA Test | ₹35,000 – ₹50,000 | Recommended only for Repeated Implantation Failure (RIF). |
Frozen Embryo Transfer | ₹40,000 – ₹60,000 | Mandatory if doing PGT-A/ERA. Includes thawing & prep. |
PRP (Intra-uterine) | ₹10,000 – ₹15,000 per session | 1-2 sessions typical for thin lining. |
Embryo Glue | ₹5,000 – ₹15,000 | Low-cost adjuvant; widely used. |
Assisted Hatching | ₹10,000 – ₹20,000 | Standard for frozen embryos in many labs. |
Functional Medicine | Variable | Diet plans, supplements, and gut testing are separate investments. |
Total Cost Implications:
A “fully loaded” cycle (IVF + ICSI + PGT-A on 4 embryos + FET) can easily exceed ₹3,50,000 to ₹4,00,000. This highlights the importance of the functional medicine approach: improving natural fertility health might reduce the need for multiple expensive cycles or high-tech add-ons.
9. Conclusion and Recommendations
The era of “one-size-fits-all” IVF is over. Patients in Mysuru today have access to world-class technologies that can manipulate life at the cellular and genetic level. However, the availability of ICSI, PGT-A, PRP, and ERA does not imply their universal necessity.
- ICSI is a non-negotiable necessity for male factor infertility but an optional expense for others.
- PGT-A offers a powerful tool for selection in older women but adds significant cost without improving cumulative yields for younger patients.
- PRP and ERA remain valuable niche tools for specific pathologies (thin lining and displaced windows) but are not silver bullets for everyone.
ARKA Anugraha Hospital stands at the forefront of a new paradigm: Integrative Reproductive Medicine. By fusing the precision of these technological add-ons with the biological optimization of functional medicine, Dr. Gaurang Ramesh and his team offer a pathway that respects both the science of the embryo and the sanctity of the patient’s overall health.
For the Patient:
- Question the “Default”: Do not accept ICSI or add-ons as standard without asking for the specific indication for your case.
- Focus on the Foundation: Before investing in a ₹50,000 ERA test, invest in your gut health, diet, and stress management. The most sophisticated add-on cannot compensate for a highly inflamed body.
- Personalize: Use the “Traffic Light” evidence system. Prioritize “Green” interventions (lifestyle, necessary ICSI) and consider “Amber” add-ons (Glue, Hatching) as low-risk boosters.
In the complex journey of fertility, knowledge is the most potent add-on of all.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
