IBS vs IBD Understanding the Difference and Why Early Diagnosis Matters

- Published on: 23/Dec/2025
- Posted By: Arka Health

Understanding the difference early is essential. A delay or error in diagnosis can either expose a patient to unnecessary medications or, conversely, allow a serious inflammatory disease to progress unchecked. This article explains IBS and IBD clearly, highlights how doctors differentiate them early, and outlines evidence-based treatment pathways.
What Is Irritable Bowel Syndrome
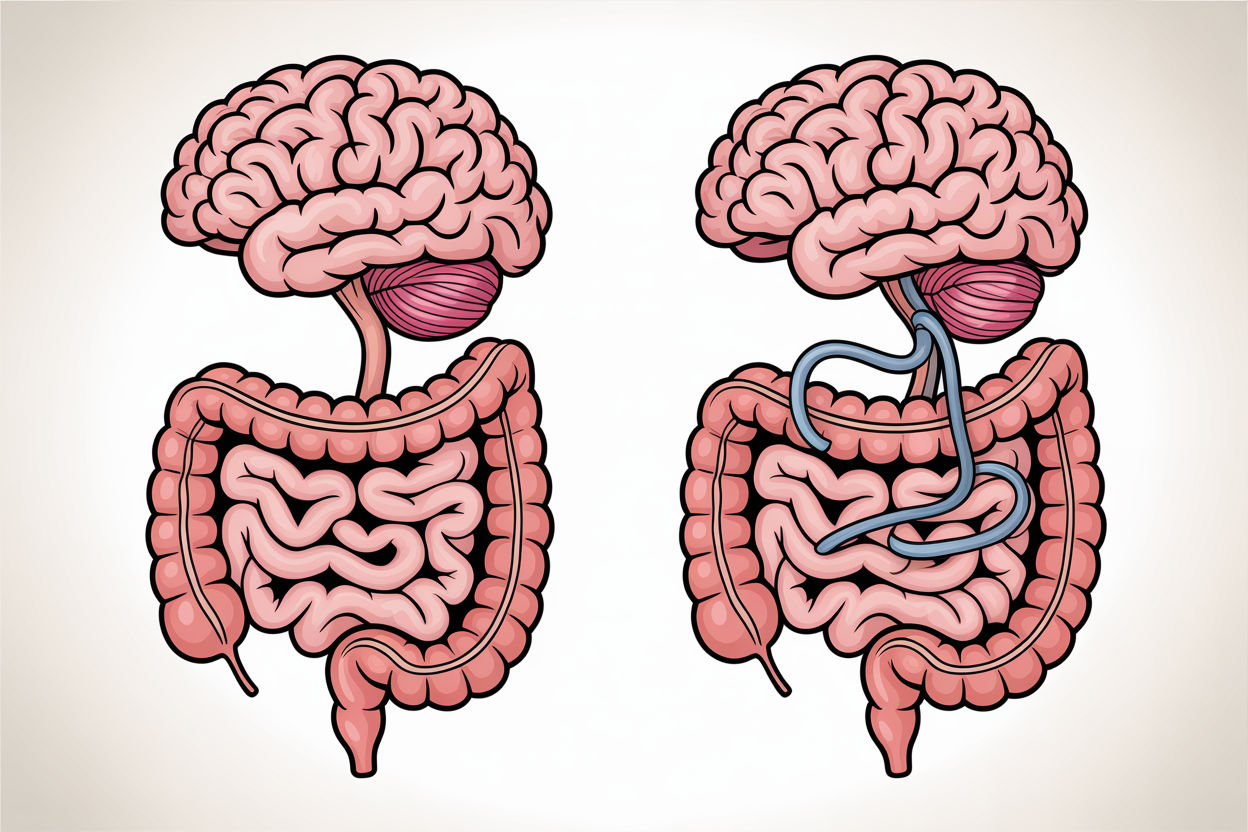
Irritable Bowel Syndrome is a disorder of gut brain interaction. It affects how the intestines function and how pain signals are processed, not the structure of the bowel itself.
In IBS, the digestive tract appears normal on scans and endoscopy, but nerve signaling, gut motility, and sensitivity are altered. This leads to symptoms that can be severe and persistent, even in the absence of visible disease.
Common IBS Symptoms
- Recurrent abdominal pain or cramping
- Bloating and abdominal distension
- Diarrhea, constipation, or alternating bowel habits
- Symptoms that worsen with stress or certain foods
- Relief of pain after passing stool in many patients
A key feature of IBS is visceral hypersensitivity. Normal gut activity is perceived as pain because the nerves lining the intestines are overly sensitive.
IBS does not cause ulcers, bleeding, tissue damage, or inflammation detectable on routine tests.
What Is Inflammatory Bowel Disease
Inflammatory Bowel Disease is a chronic immune mediated condition that causes ongoing inflammation of the digestive tract. Unlike IBS, IBD leads to visible and measurable tissue damage.
The two main forms of IBD are:
- Affects only the colon and rectum
- Inflammation is continuous and limited to the inner lining
- Common symptoms include bloody diarrhea, urgency, and rectal pain
- Can affect any part of the digestive tract from mouth to anus
- Inflammation involves the full thickness of the bowel wall
- May cause strictures, fistulas, abscesses, and nutritional deficiencies
Chronic stress reduces microcirculation to intestinal cells. This compromises oxygen delivery and weakens the protective mucus layer, increasing vulnerability to inflammation and permeability.
IBS vs IBD Key Differences at a Glance

Feature | IBS | IBD |
Nature of condition | Functional disorder | Inflammatory disease |
Inflammation | Absent | Present |
Structural damage | None | Yes |
Colonoscopy findings | Normal | Ulcers, inflammation |
Cancer risk | No | Increased with long duration |
Night symptoms | Rare | Common |
Weight loss | No | Common |
Blood in stool | No | Common |
How Doctors Differentiate IBS and IBD Early
IBS symptoms often fluctuate and are closely linked to stress, meals, or bowel movements. Symptoms usually occur during waking hours.
IBD symptoms are more persistent and may include nighttime diarrhea, fatigue, fever, and progressive worsening.
The most important early test is fecal calprotectin.
- Normal fecal calprotectin strongly supports IBS
- Elevated levels indicate intestinal inflammation and suggest IBD
Blood tests such as CRP, ESR, hemoglobin, and vitamin B12 further help identify inflammatory disease.
If inflammation markers are elevated or red flag symptoms are present, colonoscopy with biopsy is performed to confirm IBD.
IBS does not cause abnormal biopsy findings.
Red Flag Symptoms That Are Not IBS
The following symptoms should always prompt further evaluation:
- Blood in stool
- Unintentional weight loss
- Fever or night sweats
- Anemia
- Nocturnal diarrhea
- New onset symptoms after age 50
Family history of inflammatory bowel disease
Does IBS Increase the Risk of Colon Cancer
No. IBS does not increase the risk of colorectal cancer.
IBS does not cause chronic inflammation or cellular damage to the bowel lining. Patients with IBS follow standard population screening guidelines.
IBD, especially long standing ulcerative colitis and Crohn’s colitis, increases colon cancer risk due to prolonged inflammation. These patients require regular surveillance colonoscopy.
Why Symptoms May Persist Even When IBD Is in Remission
Some patients with IBD continue to experience pain, bloating, or altered bowel habits even when inflammation is controlled. This is known as functional overlay.
Causes include:
- Persistent visceral hypersensitivity
- Altered gut brain signaling
- Microbiome imbalance
- Increased intestinal permeability
- Small intestinal bacterial overgrowth
In these cases, increasing immune suppressive therapy is not helpful. Functional and integrative treatments are required.
Treatment Approach Differences
IBS Treatment Focus
- Symptom control
- Gut brain axis regulation
- Dietary modification such as low FODMAP when appropriate
- Neuromodulators for pain signaling
- Prokinetics or antispasmodics
- Stress and sleep optimization
IBD Treatment Focus
- Suppression of inflammation
- Achieving mucosal healing
- Preventing complications
- Medications such as aminosalicylates, immunomodulators, biologics
Surgery when required
Integrative Perspective on Digestive Health

Modern gastroenterology recognizes that IBS and IBD exist on a spectrum. Low grade immune activation, microbiome disruption, and intestinal permeability can influence both conditions.
An integrative approach focuses on:
- Identifying root mechanisms
- Personalised nutrition
- Microbiome support
- Nervous system regulation
- Evidence based supplementation where appropriate
How ARKA Anugraha Hospital Supports Digestive Health
At ARKA Anugraha Hospital, digestive care integrates conventional gastroenterology with functional and lifestyle-based strategies. Under the guidance of Dr Gaurang Ramesh, evaluation focuses on accurate diagnosis, mechanism-based treatment, and long term gut health rather than symptom suppression alone.
This approach is particularly valuable for patients with IBS, IBD in remission with persistent symptoms, or complex overlapping conditions.
Conclusion
IBS and IBD may appear similar on the surface, but they are fundamentally different conditions. One is a disorder of function and sensitivity, the other a disease of inflammation and tissue injury.
Early differentiation using symptom patterns and objective tests such as fecal calprotectin prevents misdiagnosis, reduces unnecessary treatments, and ensures timely care.
Understanding your condition is the first step toward effective, targeted treatment.
FAQs
Can IBS turn into IBD
No. IBS does not cause inflammation or tissue damage and does not progress into IBD. Misdiagnosis is possible if inflammatory markers are not tested early.Is IBS a psychological condition
No. IBS involves real physiological changes in gut nerve signaling, motility, and immune activation. Stress influences symptoms but does not mean the condition is psychological.Can I have IBS and IBD together
Yes. Many IBD patients in remission develop IBS-like symptoms due to nerve sensitisation and gut brain axis changes.Which test best differentiates IBS and IBD
Fecal calprotectin is the most reliable non-invasive test for distinguishing inflammatory disease from functional gut disorders.Should everyone with IBS get a colonoscopy
Not always. Colonoscopy is recommended if red flag symptoms or elevated inflammatory markers are present.Can IBS be diagnosed even if all tests are normal?
Yes. IBS is a positive clinical diagnosis based on symptom patterns and the absence of inflammatory markers. Normal tests do not mean symptoms are imagined.Is fecal calprotectin enough to rule out IBD?
In most cases, yes. A normal fecal calprotectin level has a very high negative predictive value for active IBD.Can blood tests alone detect IBD?
Blood tests can suggest inflammation but cannot confirm IBD. Endoscopy with biopsy is required for diagnosis.When should a colonoscopy be done for suspected IBS?
Colonoscopy is recommended if red flag symptoms are present or if inflammatory markers are elevated.Can imaging scans miss early IBD?
Yes. Early or mild IBD may not appear on CT or MRI scans, which is why stool markers and biopsies are important.Can IBS cause severe pain?
Yes. IBS pain can be intense due to visceral hypersensitivity, even without inflammation or damage.Does mucus in stool mean IBD?
Not necessarily. Mucus can occur in IBS due to irritation and altered motility.Is bloating more common in IBS or IBD?
Bloating is more prominent in IBS, especially when related to gut bacteria and fermentation.Can IBD symptoms fluctuate like IBS?
Yes. IBD can have flares and remission, but underlying inflammation distinguishes it from IBS.Does IBS ever cause fever?
No. Fever suggests infection or inflammation and is not typical of IBS.Does long-standing IBS ever increase cancer risk?
No. IBS does not cause chronic inflammation or cellular damage.How long does someone need IBD before cancer risk increases?
Risk typically increases after 8–10 years of extensive colonic inflammation.Do all IBD patients need frequent colonoscopy?
Surveillance depends on disease duration, extent, and activity, not just diagnosis alone.Can IBS occur after an episode of colitis or infection?
Yes. Post-infectious IBS is common after bacterial gastroenteritis.Can someone have IBS symptoms even after IBD is controlled?
Yes. This is known as functional overlay and is very common.Is functional overlay dangerous?
No, but it can significantly affect quality of life if untreated.Can IBS coexist with Crohn’s disease?
Yes. Functional symptoms can coexist even in confirmed inflammatory disease.Is fiber good or bad for IBS?
It depends on the type. Soluble fiber may help, while insoluble fiber can worsen symptoms.Should IBD patients follow a low FODMAP diet?
Low FODMAP helps symptoms but does not reduce inflammation and should be used selectively.Can diet alone cure IBD?
No. Diet supports treatment but does not replace medical therapy.Are fermented foods safe in IBS?
Some are helpful, while others may worsen symptoms depending on tolerance.Can dairy trigger IBS but not IBD?
Yes. Lactose intolerance is common in IBS and unrelated to inflammation.Why are antidepressants used in IBS?
They are used at low doses to reduce gut nerve sensitivity, not to treat depression.Are antibiotics helpful in IBS?
In selected cases such as bacterial overgrowth, specific antibiotics may help.Why can steroids be harmful if misused?
Long-term steroid use can cause bone loss, infections, and metabolic complications.Are biologic drugs lifelong in IBD?
Not always. Duration depends on disease severity, response, and relapse risk.Is IBS psychosomatic?
No. IBS involves real physiological changes in nerve signaling and immune activation.Can anxiety worsen bowel symptoms?
Yes. Anxiety affects gut motility and pain perception through the gut-brain axis.Does treating stress improve gut symptoms?
Yes. Stress management is a valid medical strategy for both IBS and IBD.Can poor sleep worsen bowel disease?
Yes. Sleep disruption affects immune regulation and gut motility.Can IBS affect work productivity?
Yes. IBS is a leading cause of absenteeism and reduced work performance.Is exercise safe in IBD?
Moderate exercise is beneficial when disease is stable.Can travel worsen IBS symptoms?
Yes. Changes in routine, food, and stress commonly trigger symptoms.Is IBS a lifelong condition?
Symptoms may fluctuate over time, and many patients achieve good control with the right approach.Can IBD go into permanent remission?
Long-term remission is possible but requires ongoing monitoring. Is early diagnosis important in IBD? Yes. Early treatment reduces complications and surgery risk.Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
