Gut Health, Sleep and Energy: The Hidden Connection

- Published on: 17/Dec/2025
- Posted By: Arka Health

Many people today feel constantly tired, struggle to sleep despite exhaustion, and experience brain fog that makes even simple tasks feel overwhelming. Blood tests are often normal. Scans show nothing alarming. Yet the fatigue persists, sleep remains disturbed, and energy never fully returns.
At ARKA Anugraha Hospital, this pattern is seen repeatedly, especially among urban populations in Bengaluru and Mysuru. Patients arrive describing digestive discomfort, poor sleep, low stamina, anxiety, and cognitive dullness, often treated as separate problems. Modern medicine now understands that these symptoms frequently arise from a single, deeply interconnected system involving the gut, the brain, circadian rhythms, immunity, and cellular energy production.
This article explains the science behind the gut-sleep-energy connection in clear, patient-friendly language. It draws directly from current research and ARKA’s integrative medical philosophy under the leadership of Dr Gaurang Ramesh, helping patients understand why these symptoms cluster together and how addressing the root connections can restore vitality.
Why Gut Health, Sleep and Energy Are Inseparable
The body does not operate as isolated organs. Digestion, sleep regulation, immune balance, and energy production are biologically interwoven. When one system becomes disturbed, the others follow.
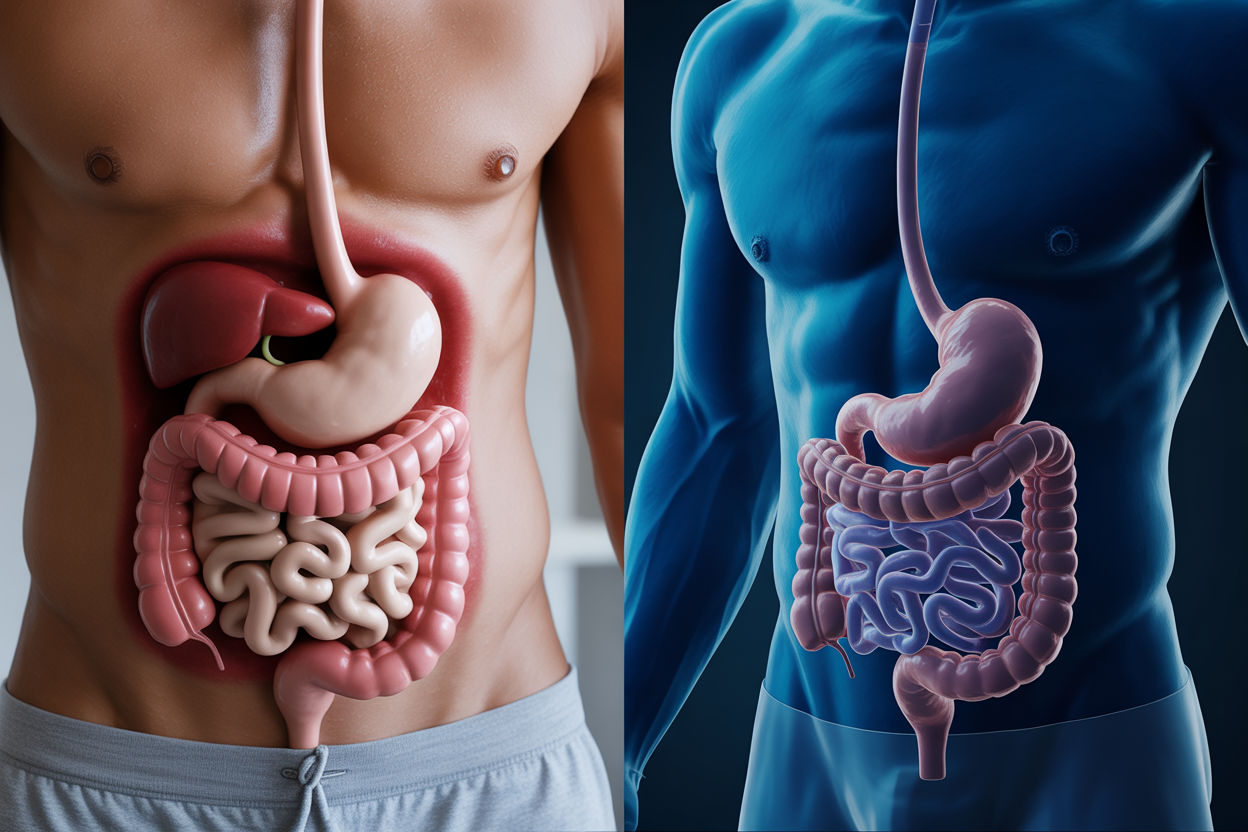
The gut plays a central role in this network because it is not only a digestive organ. It is a neurological, immune, hormonal, and metabolic command centre. Signals originating in the gut influence how deeply you sleep, how refreshed you feel in the morning, and how efficiently your cells produce energy throughout the day.
This integrated system can be understood through three major connections:
- the gut-brain axis
- circadian biology and the microbiome
- mitochondrial energy regulation
The Gut-Brain Axis: How the Gut Talks to the Brain
The gut-brain axis is the communication network linking the digestive tract to the brain. It works continuously through nerves, chemical messengers, and immune signals.
The vagus nerve connects the gut directly to the brainstem. Importantly, most of the signals travel from the gut to the brain, not the other way around. This means the brain constantly receives updates about the state of digestion, inflammation, microbial balance, and gut integrity.
When the gut environment is calm and balanced, these signals promote mental clarity, emotional stability, and relaxed sleep readiness. When the gut is inflamed, permeable, or imbalanced, the vagus nerve transmits distress signals that activate anxiety circuits in the brain, even when no external stressor is present.
This is why some people feel anxious, restless, or wired without understanding why. The source of the signal may be coming from the gut.
The gut produces most of the body’s neurotransmitters that regulate mood and sleep.
Serotonin, essential for emotional balance and sleep regulation, is largely produced in the digestive tract. Its availability directly affects sleep quality and daytime energy.
GABA, the brain’s primary calming neurotransmitter, is produced by specific gut bacteria. When these bacteria decline due to dysbiosis, the nervous system loses its natural braking system, leading to difficulty falling asleep despite fatigue.
This explains the common complaint of being “tired but wired”.
The gut houses nearly 70 percent of the immune system. When the intestinal lining becomes permeable, bacterial toxins and undigested particles enter the bloodstream. The immune system responds by releasing inflammatory chemicals.
These inflammatory molecules can cross into the brain, activating microglial cells and creating neuroinflammation. Clinically, this appears as:
- brain fog
- poor concentration
- mental fatigue
- low motivation
- disrupted sleep
This is not a psychological weakness. It is immune-driven neurological stress.
Circadian Rhythm and the Microbiome
Sleep is regulated by circadian rhythms, internal clocks that follow a roughly 24-hour cycle. What is less known is that the gut microbiome follows its own circadian rhythm, synchronised with feeding and sleep patterns.
Microbial Daily Cycles
During the day, gut bacteria involved in digestion and energy extraction dominate. At night, bacteria involved in repair, detoxification, and gut barrier maintenance become more active.
This rhythmic shift is controlled by clock genes and influenced by meal timing, sleep habits, and light exposure.
When Sleep Disruption Breaks Gut Rhythm
Poor sleep, late nights, shift work, or irregular eating disrupt microbial rhythms. This desynchronisation, often called metabolic jetlag, leads to:
- loss of beneficial bacteria
- increased gut permeability
- higher inflammation
- impaired glucose regulation
Once this cycle begins, poor sleep worsens gut health, and poor gut health further worsens sleep.
The Gut and Melatonin Production
Melatonin is the hormone that signals darkness and prepares the body for sleep. While the pineal gland releases melatonin into the bloodstream, the gut produces far larger amounts locally.
Gut-derived melatonin:
- supports intestinal motility
- protects the gut lining from oxidative stress
- reinforces barrier integrity
Dysbiosis and inflammation reduce this gut-based melatonin production, contributing to fragmented sleep and early awakenings.
The Energy Connection: Mitochondria and the Gut

Energy is produced inside cells by mitochondria. When people experience chronic fatigue that does not improve with rest, the issue often lies at the cellular level.
The Gut-Mitochondria Axis
Gut bacteria and mitochondria share evolutionary origins and communicate through metabolites. One of the most important is butyrate, a short-chain fatty acid produced by fiber-fermenting bacteria.
Butyrate supports mitochondrial efficiency, reduces oxidative stress, and signals cells to produce energy efficiently.
Low butyrate production, common in dysbiosis, leads to reduced cellular energy output.
Inflammation and the Cellular Danger Response
When bacterial toxins enter circulation due to leaky gut, mitochondria receive danger signals. In response, they intentionally slow energy production to protect the cell. This survival response is adaptive in acute illness but harmful when it becomes chronic.
Patients experience this as persistent fatigue, heaviness, poor exercise tolerance, and slow recovery.
Nutrient Absorption and Energy Deficiency
Energy production requires micronutrients like B-vitamins, magnesium, iron, and coenzyme Q10. Gut inflammation, low stomach acid, or bacterial overgrowth reduce absorption, creating functional deficiencies even when blood levels appear borderline normal.
This combination of toxin exposure and nutrient shortfall explains why many patients feel exhausted despite eating adequately.
Vitamin D: The Overlooked Regulator
Vitamin D deficiency is extremely common in India, including Karnataka. Vitamin D influences:
- gut barrier integrity
- microbiome diversity
- immune regulation
- sleep quality
Deficiency worsens inflammation, disrupts sleep architecture, and weakens energy metabolism. Absorption of Vitamin D itself depends on gut health, creating a feedback loop.
Post-Viral Fatigue and Gut Reservoirs

After viral infections, including COVID-19, some individuals experience prolonged fatigue and brain fog. Research suggests viral particles can persist in gut tissue, maintaining immune activation.
This ongoing gut-based inflammation continues to signal the brain through the vagus nerve, sustaining fatigue even after respiratory recovery.
ARKA Anugraha Hospital’s Integrative Perspective
ARKA Anugraha Hospital approaches gut, sleep, and energy as a unified system. Under the leadership of Dr Gaurang Ramesh, the focus is on identifying upstream dysfunction rather than suppressing downstream symptoms.
Integrative Modalities at ARKA
ARKA combines conventional gastroenterology with integrative therapies that support nervous system balance, immune regulation, and cellular energy.
These include:
- Functional gastroenterology
- Ayurveda
- Yoga and Yoga Nidra
- Sound-based therapies
- Ozone therapy as part of integrative care
These approaches are used responsibly and as complements, not replacements, to standard medical evaluation.
Traditional Nutrition and Energy Regulation
Fermented Foods
Traditional South Indian foods like idli and dosa, when prepared traditionally, provide natural probiotics that support digestion and nutrient absorption.
Fermentation improves mineral bioavailability and supports microbial diversity.
Ragi and Energy Stability
Ragi supports stable blood sugar, provides calcium required for melatonin synthesis, and supplies prebiotic fiber that feeds butyrate-producing bacteria. This contributes to sustained energy and better sleep maintenance.
Recognising a Gut-Sleep-Energy Pattern
Patients often experience symptoms across multiple domains:
- digestive discomfort
- disturbed sleep
- brain fog
- reliance on caffeine
- low stamina
When these occur together, it strongly suggests an underlying gut-brain-energy imbalance.
Restoring Rhythm, Not Chasing Symptoms

Gut health, sleep quality, and energy production are deeply interconnected. Chronic fatigue and insomnia are rarely isolated problems. They are signals of disrupted communication between the gut, brain, immune system, and mitochondria.
At ARKA Anugraha Hospital, the goal is to restore rhythm and resilience across these systems. By addressing root connections rather than isolated symptoms, patients can move from constant exhaustion to sustained vitality.
Frequently Asked Questions
Q1. Why do I feel tired even after sleeping for 7 – 8 hours?
Sleep duration alone does not guarantee restorative sleep. Inflammation, poor gut health, and disrupted circadian rhythms can prevent deep sleep stages needed for recovery.
Q2. Can gut issues really affect my sleep?
Yes. The gut produces neurotransmitters and melatonin precursors. Dysbiosis and inflammation directly interfere with sleep regulation.
Q3. What is brain fog and why does it happen with gut problems?
Brain fog is a result of neuroinflammation, immune activation, and mitochondrial slowdown driven by gut-derived inflammatory signals.
Q4. Is chronic fatigue always psychological?
No. Chronic fatigue often reflects cellular energy suppression caused by inflammation, nutrient malabsorption, and mitochondrial stress.
Q5. Why do stress and poor sleep worsen digestion?
Stress hormones reduce blood flow and enzyme production in the gut, while poor sleep disrupts microbial balance and gut barrier repair.
Q6. How long does recovery usually take?
Restoring gut-sleep-energy balance is a gradual biological process. Improvements often occur over weeks to months with consistent care.
Q7. Does ARKA treat fatigue differently from conventional clinics?
ARKA evaluates fatigue as a systems issue involving gut health, sleep biology, immunity, and energy metabolism rather than a single symptom.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
