Gut Brain Axis: How Anxiety and Mood Influence Your Digestion

- Published on: 16/Dec/2025
- Posted By: Arka Health
If you live in a fast-paced city like Bangalore, you may have experienced this: you feel bloated, uneasy, or rushed to the bathroom during work stress. You finish an endoscopy, ultrasound, and blood tests, and everything comes back normal. Yet your discomfort is real.
This gap between normal test results and persistent symptoms is one of the strongest clues that the gut brain axis is involved.
The gut brain axis explains why emotional stress, thoughts, and even a bad day at work can change how your stomach feels. It describes how your gut and brain talk to each other every second using nerves, hormones, microbes, and chemical messengers. When this communication becomes strained, digestion reacts immediately.
This guide simplifies a very complex system into a clear, readable explanation, so patients understand what is happening inside their bodies and why these symptoms are not imaginary.
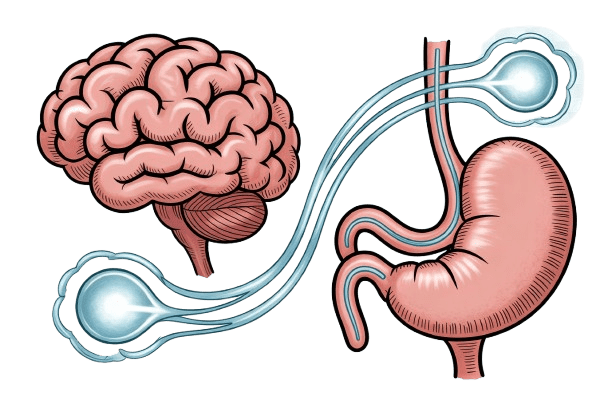
What Exactly Is the Gut Brain Axis
The gut brain axis is a two-way communication network linking your digestive system and your brain. Think of it as a constant conversation. When something affects your mood, your gut listens. When something irritates your gut, your brain reacts.
This is why you feel:
- butterflies before an exam
- a sinking feeling during bad news
- a tight stomach during anxiety
- bloating or urgency before stressful meetings
This is biology, not imagination.
Three major systems make this communication possible.
The Enteric Nervous System: Your Second Brain
The gut has its own nervous system called the enteric nervous system. It contains hundreds of millions of neurons. This is why scientists call it the second brain.
It controls:
- movement of food
- release of digestive juices
- blood flow inside the gut
- sensation of pain, fullness, and pressure
The incredible part is that the enteric nervous system can function on its own. Even if it were disconnected from the brain, it could still move food and coordinate basic digestion. But under normal conditions, it constantly talks to the main brain to keep everything balanced.
The Vagus Nerve: The Main Communication Line
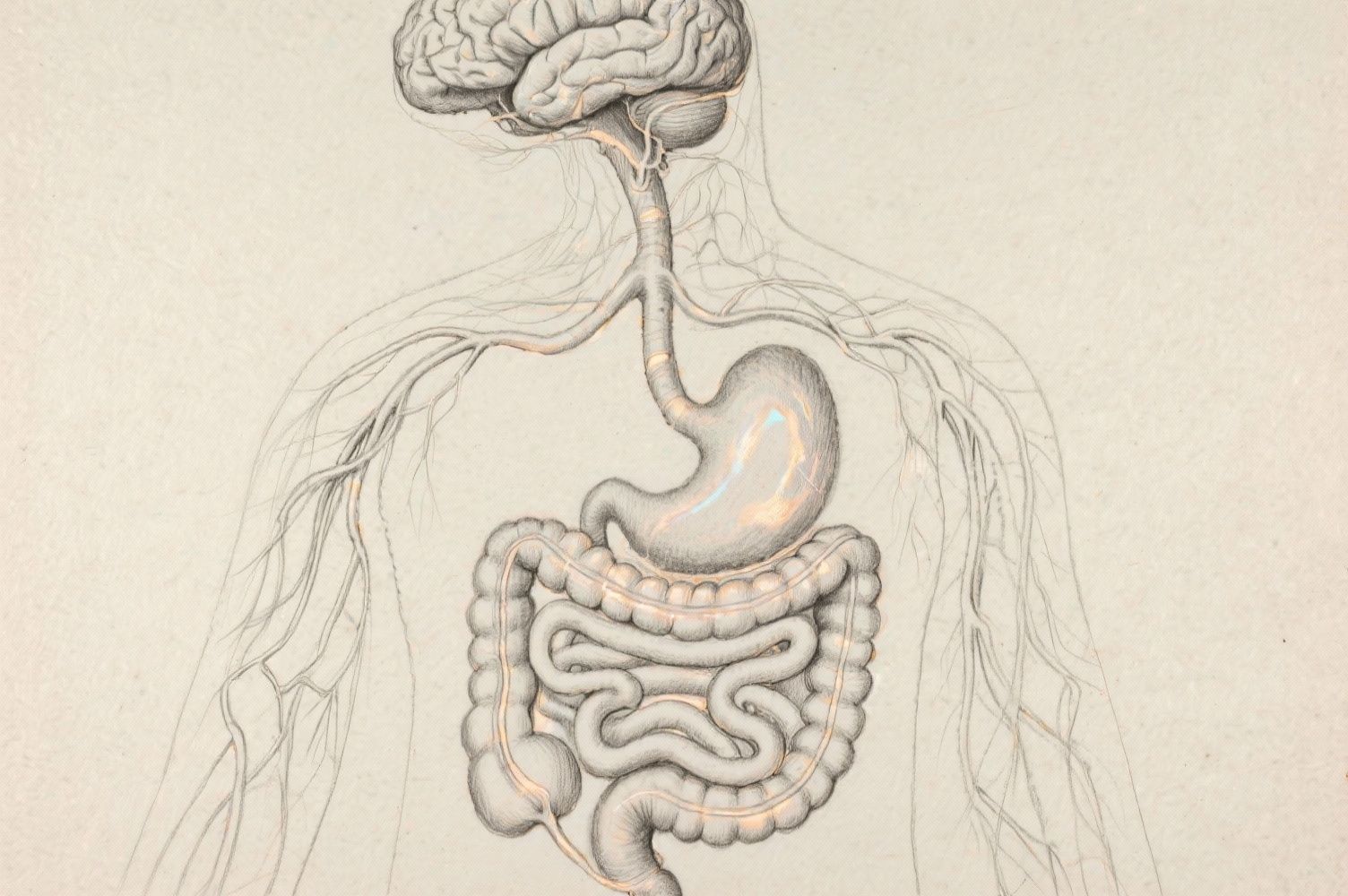
The vagus nerve connects the brainstem to the stomach and intestines. What surprises most people is that most of the signals travel upward from the gut to the brain.
This means your brain understands what is happening in your gut before you consciously notice symptoms.
High vagal tone (healthy communication) supports:
- calm digestion
- steady motility
- balanced acid and enzyme release
- stable mood
Low vagal tone, often caused by stress, results in:
- bloating
- constipation
- nausea
- increased anxiety
- poor gut repair
When people say stress gets “stuck in the stomach,” the vagus nerve is usually involved.
The HPA Axis: How Stress Alters Digestion

The hypothalamic pituitary adrenal axis is the body’s hormonal stress response. When you feel threatened, overworked, or emotionally overwhelmed, your brain activates this pathway and releases cortisol.
Cortisol helps you survive danger, but it harms digestion.
High cortisol:
- reduces blood flow to the digestive organs
- slows stomach emptying
- weakens the gut lining
- changes the microbiome
- increases sensitivity to pain
This is why many people experience stomach problems during busy work periods, relationship stress, or emotional strain.
Over time, the stress response becomes chronic. This keeps the gut in a defensive mode instead of a digestive mode.
Neurotransmitters: How Chemicals Link Mood and Digestion
Your gut produces many of the same neurotransmitters that regulate mood. These chemicals explain why emotional health is tightly linked to digestive health.
Around 95 percent of the body’s serotonin is made in the gut. Serotonin controls:
- how fast food moves
- how sensitive the gut feels
- how much fluid the gut releases
If serotonin signalling is too high, diarrhea may occur. If it is too low, constipation becomes more likely. This variation explains why IBS can look different from person to person.
Because antidepressants act on serotonin, they often cause nausea, loose stools, or constipation.
Dopamine helps the stomach relax and protects the gut lining. If dopamine levels are disrupted, patients may experience heaviness, early fullness, or discomfort after eating.
Some gut bacteria produce GABA, a calming neurotransmitter. When GABA-producing microbes decrease due to stress or poor diet, anxiety levels rise and digestive rhythm becomes irregular.
The Microbiome and the Gut Brain Connection

Trillions of microbes live inside you. They help digest food, protect the gut lining, and produce chemicals that influence your brain.
Short Chain Fatty Acids: Microbial Messages
When good bacteria ferment fiber, they create short chain fatty acids like butyrate. Butyrate is like fuel for your colon and plays a big role in reducing inflammation.
Low SCFA levels increase the risk of:
- anxiety
- poor gut barrier function
- brain fog
- increased pain sensitivity
Tryptophan and Mood
The microbiome decides how tryptophan, an amino acid, is used. When gut balance is healthy, tryptophan becomes serotonin. When the gut is inflamed, tryptophan shifts into pathways linked to low mood.
Dysbiosis: When Gut Bacteria Lose Balance
Stress, infections, antibiotics, poor sleep, or processed foods can reduce microbial diversity. This imbalance increases inflammatory chemicals that travel through the bloodstream and influence brain regions linked to fear and stress response.
This is one of the major reasons anxiety and gut symptoms occur together.
How Stress Physically Changes Digestion
Stress is not just a feeling. It creates real, measurable changes inside your digestive system.
During stress, the body diverts blood to the muscles and brain. The gut receives less oxygen and fewer nutrients, which slows healing and causes indigestion.
This results in:
- heaviness
- gas
- poor breakdown of food
slower motility
Stress lowers stomach acid and digestive enzymes. Food is not broken down properly, leading to:
- fermentation
- bloating
discomfort after meals
Stress affects different parts of the gut in different ways.
- The stomach empties more slowly.
- The intestine may speed up or slow down.
- The colon becomes more sensitive.
This is why some people experience diarrhea during stress, while others feel constipated or unable to empty fully.
Chronic stress lowers the threshold for pain. Normal gas or stretching of the gut becomes uncomfortable or painful. The brain interprets routine sensations as threats.
This is one of the strongest explanations for why IBS pain feels so sharp even when tests are normal.
Stress weakens tight junctions between cells in the gut lining. Undigested particles and bacterial fragments enter the bloodstream, triggering inflammation. This inflammation affects both mood and digestion.
People often report:
- bloating
- fatigue
- poor concentration
- increased anxiety
Common Conditions Related to the Gut Brain Axis
Many patients who visit ARKA Anugraha Hospital with persistent digestive symptoms fall into one of these categories.
IBS: The Classic Gut Brain Axis Disorder
IBS is not a structural disease. It is a communication disorder of the gut brain axis.
Common symptoms:
- alternating constipation and diarrhea
- abdominal pain
- urgency during stress
- bloating
Around 40 to 60 percent of IBS patients also experience anxiety. This is because stress alters motility and serotonin signalling, while gut discomfort increases stress.
Functional Dyspepsia
Symptoms include:
- upper abdominal discomfort
- early fullness
- nausea
- bloating after small meals
Stress slows stomach relaxation and increases sensation, making these symptoms worse.
SIBO Patterns Linked to Stress
Chronic stress slows the migrating motor complex, a cleansing wave that moves through the small intestine during fasting. When this slows down, bacteria accumulate. This leads to:
- bloating
- pressure
- distention after meals
GERD and Stress Sensitivity
Stress does not always increase acid. Instead, it increases how strongly you feel acid. A mild reflux episode becomes painful when the nervous system is sensitised.
Why Bangalore Shows High Rates of Gut Brain Axis Issues
Bangalore’s modern lifestyle forms the perfect environment for gut brain axis disruption:
- long commutes
- irregular meals
- late-night work schedules
- high pressure jobs
- screen overuse
- disturbed sleep
- processed food habits
Surveys show nearly 70 percent of urban Indians experience digestive issues. A large portion of this is linked to chronic stress and lifestyle demands rather than structural disease.
At ARKA Anugraha Hospital, we frequently meet young professionals who have normal test results but severe bloating, irregular stools, or burning sensations. Understanding the gut brain axis helps them recognise that their symptoms are real and scientifically explained.
Your Gut Is Talking to You
The gut brain axis is one of the most important systems in the body. It explains why stress affects digestion and why digestive issues affect mood. When this communication becomes disrupted, symptoms appear even when scans or tests are normal.
Your gut is not failing. It is sending signals.
At ARKA Anugraha Hospital, we help patients understand these signals with clarity and compassion. The goal is not only to interpret symptoms but to help you regain confidence in your own body. When the gut brain axis is understood, patients stop blaming themselves and start recognising patterns that can be addressed with the right guidance.
Your gut and brain are partners. When they communicate well, you feel well.
Expanded FAQs on the Gut Brain Axis
Q1. Can stress really cause stomach problems, or is it just psychological?
Yes, stress can cause very real physical stomach symptoms. When you feel stressed, your brain activates the sympathetic nervous system. This reduces blood flow to the gut, slows digestion, reduces stomach acid and enzymes, and makes the intestines contract irregularly. These physical changes cause gas, bloating, pain, constipation, or diarrhea.
None of this is imagined. It is a biological response created by the gut brain axis.
Q2. Why do my tests look normal even though my symptoms are severe?
Most gut brain axis problems are functional, not structural.
Scans and blood tests look for ulcers, cancers, infections, or inflammation. In gut brain axis disorders, the structure of the gut is normal. The issue lies in how the gut and brain communicate.
This means your symptoms can be intense even when imaging and labs look perfect.
Q3. Why do I get diarrhea or constipation during stressful situations?
Stress changes gut motility.
When you are anxious, the brain sends signals that speed up activity in the colon. This causes urgency or diarrhea.
With long term stress, the opposite can happen. Vagal tone drops and the colon slows down, leading to constipation.
Your bowels are reacting to your emotional state.
Q4. Why does bloating get worse when I am anxious?
Anxiety increases something called visceral hypersensitivity.
This means the nerves in your gut become extra sensitive. Normal gas or movement feels more uncomfortable than usual.
Stress also reduces digestion quality, leading to more fermentation and gas production. The combination creates intense bloating.
Q5. How does the vagus nerve affect my digestion and anxiety?
The vagus nerve is the main pathway connecting your gut and brain.
When it works well, digestion feels smooth and your body feels calm.
When it becomes weak due to stress, digestion slows, inflammation rises, and your anxiety levels increase.
The vagus nerve is like a communication bridge. If the bridge weakens, both sides are affected.
Q6. What does it mean when people say the gut is the second brain?
Your gut has its own nervous system with hundreds of millions of neurons. It makes decisions on motility, enzyme release, and blood flow without waiting for the brain. It also produces neurotransmitters like serotonin and dopamine. In this way, the gut behaves like a second brain with power to influence mood, digestion, and even immunity.
Q7. Why do I feel a lump in my throat, tightness in my stomach, or nausea during emotional stress?
These sensations come directly from the gut brain axis. When stress hormones rise, the stomach and intestines slow down or spasm. Blood is diverted away from the digestive system, and the vagus nerve becomes overstimulated. This creates feelings of tightness, loss of appetite, nausea, or butterflies.
Q8. Can my gut bacteria really affect how I feel emotionally?
Yes. Gut bacteria produce chemicals that influence the brain.
For example:
- Some bacteria make GABA, a calming neurotransmitter.
- Others influence serotonin production.
- Fiber-fermenting bacteria create short chain fatty acids that reduce inflammation.
When the microbiome is imbalanced, anxiety, irritability, and digestive discomfort can increase.
Q9. What is a leaky gut and how is it connected to mood and anxiety?
Leaky gut refers to increased permeability of the intestinal lining.
Stress hormones weaken this barrier, allowing toxins and bacterial fragments to enter the bloodstream.
These fragments trigger immune reactions and inflammation, which can travel to the brain and worsen anxiety, fatigue, and mood swings.
Q10. Why does my stomach hurt when I am nervous, even if I have not eaten anything?
Pain during stress occurs due to heightened nerve sensitivity.
Your brain becomes hyper-alert during anxiety. It amplifies signals from the gut, making normal contractions or movement feel painful.
This is visceral hypersensitivity, a core feature of gut brain axis disorders like IBS.
Q11. Why do people with IBS often have anxiety (and vice versa)?
IBS is strongly linked to anxiety because both conditions involve altered serotonin signalling and nervous system sensitivity.
Anxious states change gut motility and sensation.
Unpredictable bowel habits increase worry and fear of symptoms.
This creates a loop where gut symptoms worsen anxiety, and anxiety worsens gut symptoms.
Q12. Is there a structural problem in my gut when the gut brain axis is disrupted?
Usually no. Gut brain axis disorders involve functional changes, not structural damage.
The gut walls, tissues, and organs often appear normal in tests. The issue lies in nerve sensitivity, communication pathways, microbiome balance, and stress response.
Q13. Why does Bangalore’s lifestyle make gut issues worse?
Bangalore’s high stress environment affects the gut brain axis through:
- irregular eating patterns
- long commute times
- heavy workload
- late nights and screen exposure
- reduced sleep quality
- processed food intake
These factors weaken vagal tone, disrupt the microbiome, and increase inflammation, making gut symptoms more common.
Q14. Can mood improve when gut health improves?
Yes. Since the gut produces most of your serotonin and communicates constantly with the brain, improving gut balance often reduces anxiety, irritability, and brain fog. The gut brain axis works both ways. When one heals, the other benefits.
Q15. Why do I feel brain fog, fatigue, or difficulty concentrating along with my digestive issues?
These are side effects of inflammation and altered neurotransmitter signalling.
When the gut is inflamed or permeable, inflammatory molecules and toxins enter the bloodstream. These can affect brain function, creating foggy thinking and reduced focus.
Q16. Is my gut problem all in my head?
Absolutely not. Your symptoms are physical responses to stress hormones, nerve sensitivity, microbial changes, and vagus nerve signalling. The gut brain axis is a biological system. Problems in this system produce real, measurable changes, even if tests come back normal.
Q17. Can the gut brain axis explain why symptoms come and go?
Yes. Stress levels fluctuate. Sleep patterns change. Hormones shift. Microbiome composition varies day to day. Because the gut brain axis is constantly adapting, symptoms may be worse during stressful periods and better during calm phases.
Q18. Should I be worried if my gut issues are linked to stress?
No, you should not be worried. Stress related gut issues are extremely common, especially in busy urban settings. Understanding the gut brain axis helps you recognise that your body is reacting predictably, not failing.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
