Functional Dyspepsia Explained (Normal Tests but Persistent Symptoms)

Published on: 09/Dec/2025
Posted By: Arka Health
Introduction: The Frustration of "Everything Looks Normal"
Imagine this scenario: You have been suffering from a burning sensation in your upper abdomen for months. You feel full after eating just a few bites of your lunch. You finally visit a gastroenterologist in Bangalore, undergo an endoscopy, and wait anxiously for the results. The doctor walks in and says, “Good news, your report is completely normal. It’s just mild gastritis.”
But you don’t feel normal. The pain is real, the bloating is uncomfortable, and the chronic indigestion is affecting your work and sleep.
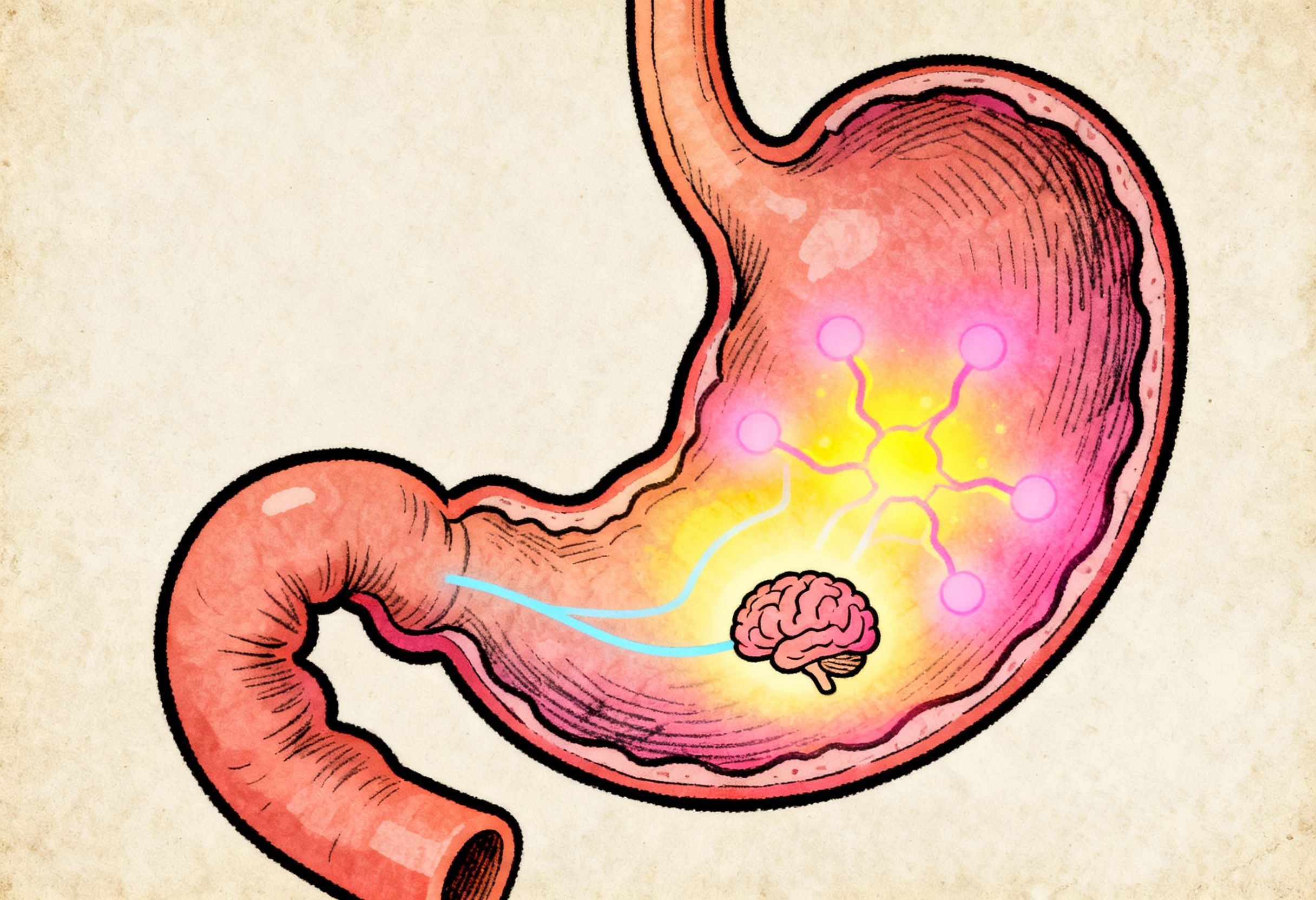
This is the most common narrative we hear at Arka Anugraha Hospital. You are likely suffering from Functional Dyspepsia (FD). It is a condition where the “hardware” of your stomach (the structure) looks fine, but the “software” (the function) is glitching. It is not “all in your head”, it is a very real physiological disorder of the gut-brain interaction.
In this guide, we will decode this complex condition, explain why your tests are normal, and explore the most effective functional dyspepsia treatment options available in Bangalore under the guidance of Dr. Gaurang Ramesh.
What is Functional Dyspepsia?
Defining the “Invisible” Illness
Functional Dyspepsia is a chronic disorder of sensation and movement (peristalsis) in the upper digestive tract. According to the Rome IV criteria (the global standard for diagnosing gut disorders), it is defined by the presence of symptoms like upper abdominal discomfort, burning, or fullness for at least three months, with no structural abnormalities found on routine tests like endoscopy.
Simply put, your stomach is structurally sound, no ulcers, no tumors, no severe inflammation but it is hypersensitive and struggling to digest food efficiently.
The Two Faces of Functional Dyspepsia
Not all indigestion is the same. FD is generally categorized into two subtypes, though many patients in Bangalore experience an overlap of both:
- Postprandial Distress Syndrome (PDS): This is meal-related. You feel uncomfortably full immediately after starting a meal (early satiety) or experience heavy bloating that lasts for hours after eating.
- Epigastric Pain Syndrome (EPS): This is characterized by burning stomach pain or aching in the upper abdomen that can occur even on an empty stomach. It is often mistaken for acidity or ulcers.
Why Do I Have This? (The Root Causes)

If there is no ulcer, what is causing the pain? Functional Dyspepsia is a multifactorial condition, meaning several triggers come together to create the perfect storm in your gut.
Visceral Hypersensitivity
This is the hallmark of FD. The nerves lining your stomach are hypersensitive. Normal amounts of gas or acid, which wouldn’t bother an average person, are interpreted by your brain as severe pain or upper abdominal discomfort. Your pain threshold is lowered, often due to past infections or chronic stress.
Impaired Gastric Accommodation
Normally, when you eat, the upper part of your stomach relaxes and expands to accommodate the food. In many FD patients, the stomach remains stiff and rigid. This forces food down too quickly or creates high pressure, leading to early satiety, the feeling that you are “stuffed” after just half a distinct roti or idli.
Delayed Gastric Emptying (Gastroparesis Lite)
In about 30% of patients, the stomach muscles are sluggish. Food sits in the stomach longer than it should, fermenting and causing chronic indigestion, nausea, and belching.
The Bangalore Stress Factor
The IT capital of India is also the stress capital. The “Gut-Brain Axis” is a direct hotline between your emotional state and your digestion. High stress (common in tech professionals with erratic deadlines) keeps the body in “fight or flight” mode. This shuts down digestion, reduces blood flow to the gut, and amplifies pain signals. At Arka Anugraha Hospital, we often see FD flare-ups correlate directly with high-stress project deliveries.
Diagnosis - Why the "Normal" Test Matters

The Role of Endoscopy
When you search for functional dyspepsia treatment, the first step is often an endoscopy. Its primary purpose is exclusion. We need to ensure there are no peptic ulcers, H. pylori infections, or malignancies. A negative endoscopy is actually a positive step, it confirms that your stomach lining is intact.
H. Pylori Testing
Helicobacter pylori is a common bacterial infection in India. It can mimic FD symptoms. We always test for this because eradicating H. pylori can sometimes cure dyspepsia. However, if the bacteria are gone and pain persists, the diagnosis is confirmed as Functional Dyspepsia.
The Arka Difference: Functional Testing
While most clinics/Hospitals stop at endoscopy, Dr. Gaurang Ramesh digs deeper. Since FD is a functional issue, we may look at:
- Food Intolerance Testing: To see if specific foods (like gluten or dairy) are triggering low-grade inflammation.
- SIBO Breath Tests: Small Intestinal Bacterial Overgrowth can often mimic FD symptoms like bloating and early satiety.
Functional Dyspepsia Treatment Options
Treating FD requires a shift from “suppressing acid” to “restoring function.” At Arka Anugraha Hospital, we employ a holistic protocol that blends modern medical gastroenterology with functional medicine principles.
Medical Management (Conventional)
- Acid Suppression: Proton Pump Inhibitors (PPIs) like Pantoprazole or Rabeprazole may be used for a short course if burning stomach pain is the dominant symptom.
- Prokinetics: Drugs like Itopride or Levosulpiride help “kickstart” the stomach muscles, aiding gastric emptying and relieving that heavy, brick-in-the-stomach feeling.
- Neuromodulators: Since the gut nerves are hypersensitive, low-dose tricyclic antidepressants are sometimes used to dampen pain signals sent to the brain. This is not for depression, but for “visceral analgesia”.
The Functional Medicine Approach (The 5R Protocol)
Dr. Gaurang Ramesh emphasizes treating the person, not just the pain.
- Remove: Eliminate triggers. Common culprits in the Indian diet include excessive chili, fried snacks, and coffee on an empty stomach.
- Replace: If stomach acid is actually low (common in chronic stress), we may need to support digestion with enzymes rather than suppressing acid.
- Repair: Using nutrients like Zinc Carnosine and L-Glutamine to soothe the mucosal lining and reduce upper abdominal discomfort.
- Rebalance: Restoring the gut microbiome with specific probiotics that reduce bloating.
- Re-regulate: Managing the vagus nerve through stress-reduction techniques.
Diet for Chronic Indigestion
There is no single “FD Diet,” but specific changes help:
- Eat Small, Frequent Meals: Don’t overload the stomach. Eat 5 small meals instead of 3 large ones.
- Texture Matters: Soft, cooked foods (like Khichdi or Idli) are easier to digest than raw salads or heavy curries.
- Timing: Finish dinner at least 3 hours before bed to prevent night-time fullness.
Home Remedies and Lifestyle Management

While professional functional dyspepsia treatment is crucial, daily habits play a massive role in recovery.
Indian Home Remedies that Work
- Fennel Water (Saunf): Excellent for reducing bloating and aiding digestion after meals.
- Ginger Tea: A natural prokinetic that helps empty the stomach and reduce nausea.
- Buttermilk (Chaas): With a pinch of roasted cumin (Jeera) and hing (asafoetida), this is soothing and provides probiotics.
Stress Management
Since FD is a disorder of gut-brain interaction, calming the mind soothes the gut.
- Diaphragmatic Breathing: Deep belly breathing for 5 minutes before meals activates the parasympathetic nervous system (“rest and digest”).
- Yoga: Specific asanas like Vajrasana (Thunderbolt Pose) after meals can improve blood flow to the digestive organs.
Why Choose Arka Anugraha Hospital?

When dealing with chronic indigestion that doesn’t show up on tests, you need a doctor who looks beyond the scope.
- Expert Leadership: Dr. Gaurang Ramesh is unique in Bangalore, holding qualifications in both Surgical Gastroenterology and Functional Medicine. He understands anatomy and physiology.
- Integrative Care: We don’t just prescribe pills. We integrate nutrition, lifestyle coaching, and stress management into your functional dyspepsia treatment plan.
- Patient-Centric: We understand the frustration of being told “you are fine” when you are in pain. We listen, validate, and investigate until we find the root cause.
Relief is Possible
You do not have to live with the fear of eating or the constant nagging of a burning stomach. Functional Dyspepsia is a complex condition, but with the right combination of medical expertise and lifestyle adjustments, it is highly manageable.
At Arka Anugraha Hospital, we are committed to turning your “normal” test results into a “normal” life, free from pain and full of vitality.
Stop suffering in silence. Book your consultation with Dr. Gaurang Ramesh today.
Frequently Asked Questions (FAQ)
Q: What is the best functional dyspepsia treatment available in Bangalore?
A: The best treatment involves a combination of medical management (prokinetics, acid reducers) and lifestyle changes. At Arka Anugraha Hospital, Dr. Gaurang Ramesh uses an integrative approach that includes the 5R protocol, stress management, and dietary customization to treat the root cause of functional dyspepsia treatment.Q: Why is my endoscopy normal if I have severe stomach pain?
A: A normal endoscopy means you don’t have ulcers or tumors (structural diseases). However, you likely have Functional Dyspepsia, which is a problem with how the stomach functions, specifically nerve hypersensitivity and motility issues. The pain is real, even if the organ looks normal.Q: Can stress cause chronic indigestion and a burning stomach?
A: Yes, stress is a major trigger. The gut and brain are connected via the Vagus nerve. High stress keeps your body in ‘fight or flight’ mode, which slows down digestion and makes stomach nerves more sensitive to pain, leading to burning and chronic indigestion.Q: What foods should I avoid for functional dyspepsia?
A: Patients should typically avoid fatty/fried foods, excessive chili, coffee, alcohol, and carbonated drinks. Large meals can also trigger symptoms. It is best to eat small, frequent meals consisting of easily digestible foods like cooked rice, idli, and steamed vegetables.Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
