Food Sensitivities Causing IBS-Like Symptoms
The Silent Epidemic in Indian Gastrointestinal Health

- Published on: 27/Dec/2025
- Posted By: Arka Health
Introduction: Why many IBS cases are actually immune reactions
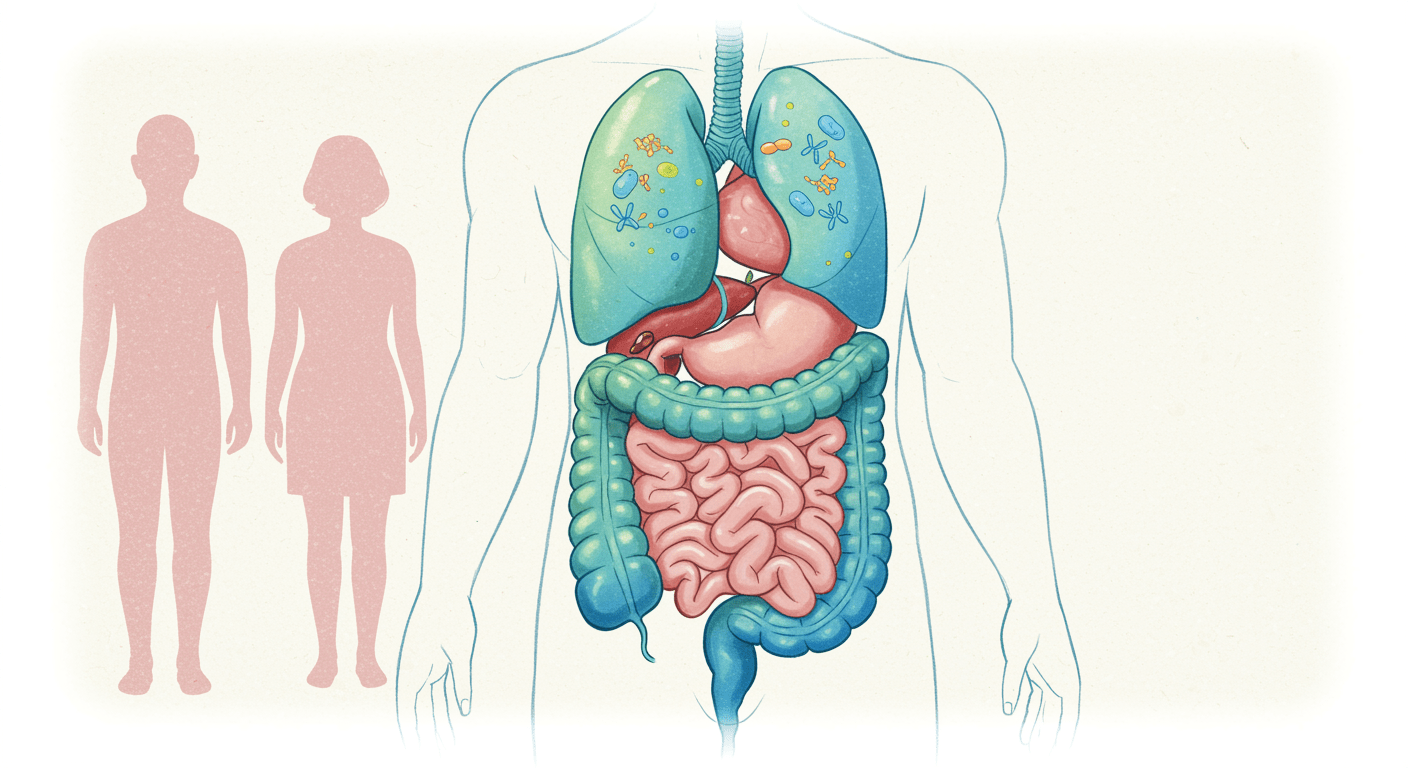
Across India, especially in urban and semi-urban regions, a growing number of patients live with chronic digestive discomfort. Bloating after meals, unpredictable bowel movements, abdominal pain, fatigue, headaches, and skin issues are often grouped under a single label: irritable bowel syndrome. While IBS is a legitimate functional diagnosis, it frequently becomes a placeholder when routine scans and blood tests appear normal.
What is increasingly clear in clinical practice is that many of these IBS-like symptoms are not purely functional. They are immune-mediated reactions to food proteins entering the bloodstream through a compromised gut barrier. These reactions are known as food sensitivities.
Unlike food allergies, food sensitivities do not cause immediate or dramatic reactions. Instead, they produce delayed, chronic inflammation that affects the gut, brain, skin, joints, and metabolism. In the Indian dietary context, where lentils, wheat, dairy, spices, and fermented foods are consumed daily, these reactions often go unnoticed for years.
This article explains how food sensitivity symptoms develop, why they mimic IBS, and how gut barrier dysfunction lies at the centre of the problem. It also outlines a clinically practical elimination and reintroduction approach adapted for Indian diets.
Understanding food sensitivities versus IBS
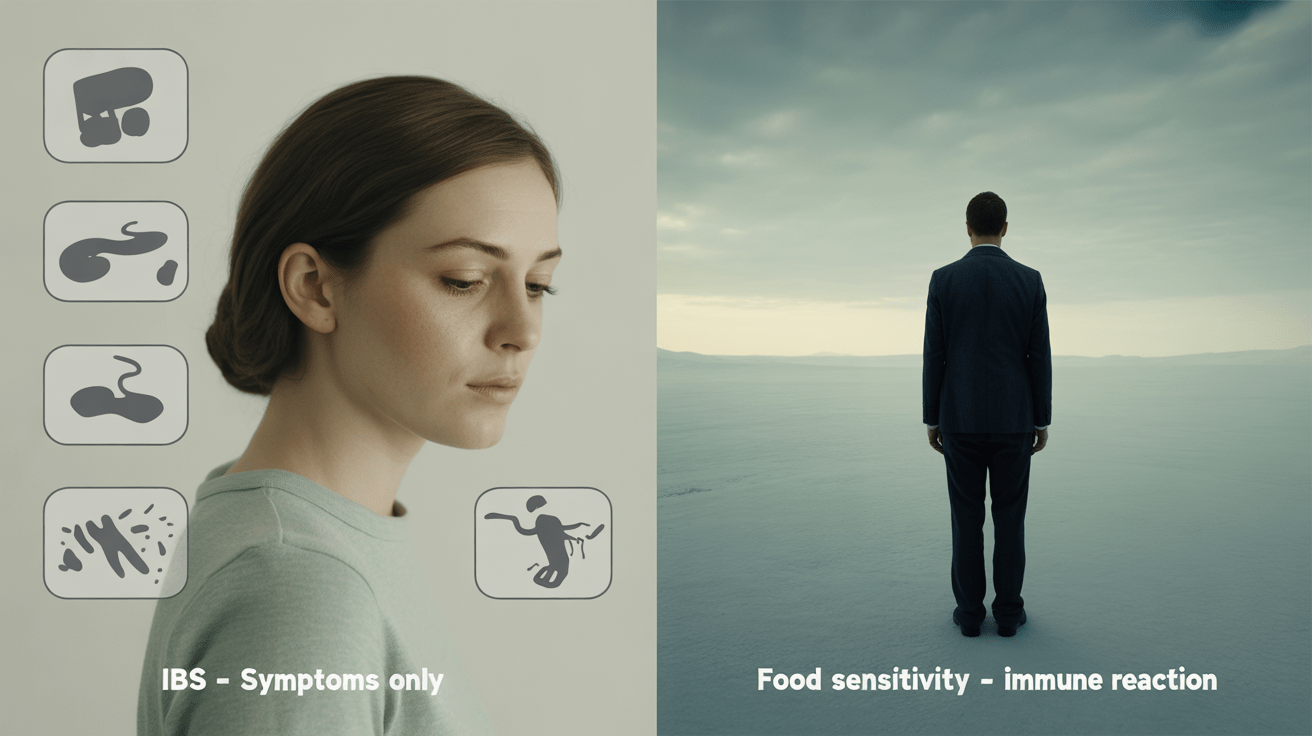
IBS is defined by symptoms, not by cause. It describes a pattern of abdominal pain associated with changes in bowel habits, without structural disease. Food sensitivities, on the other hand, are driven by immune activation.
In many patients, IBS is the outward expression of deeper processes such as intestinal permeability, immune dysregulation, and microbial imbalance. Treating IBS without addressing these mechanisms often leads to partial or temporary relief.
Food sensitivity symptoms typically include:
- Bloating and abdominal distension after meals
- Alternating diarrhoea and constipation
- Acid reflux or nausea
- Brain fog, fatigue, or migraines
- Skin conditions such as eczema or acne
- Joint stiffness or muscle aches
The delayed nature of these reactions makes them difficult to trace back to food. Symptoms may appear 24 to 72 hours after consumption, breaking the obvious cause-effect relationship.
The immune system and adverse food reactions
IgE reactions are immediate and potentially life-threatening. They cause hives, swelling, breathing difficulty, or anaphylaxis within minutes. These are detected through skin prick tests or serum IgE testing. Most patients with chronic IBS-like symptoms do not have IgE allergies.
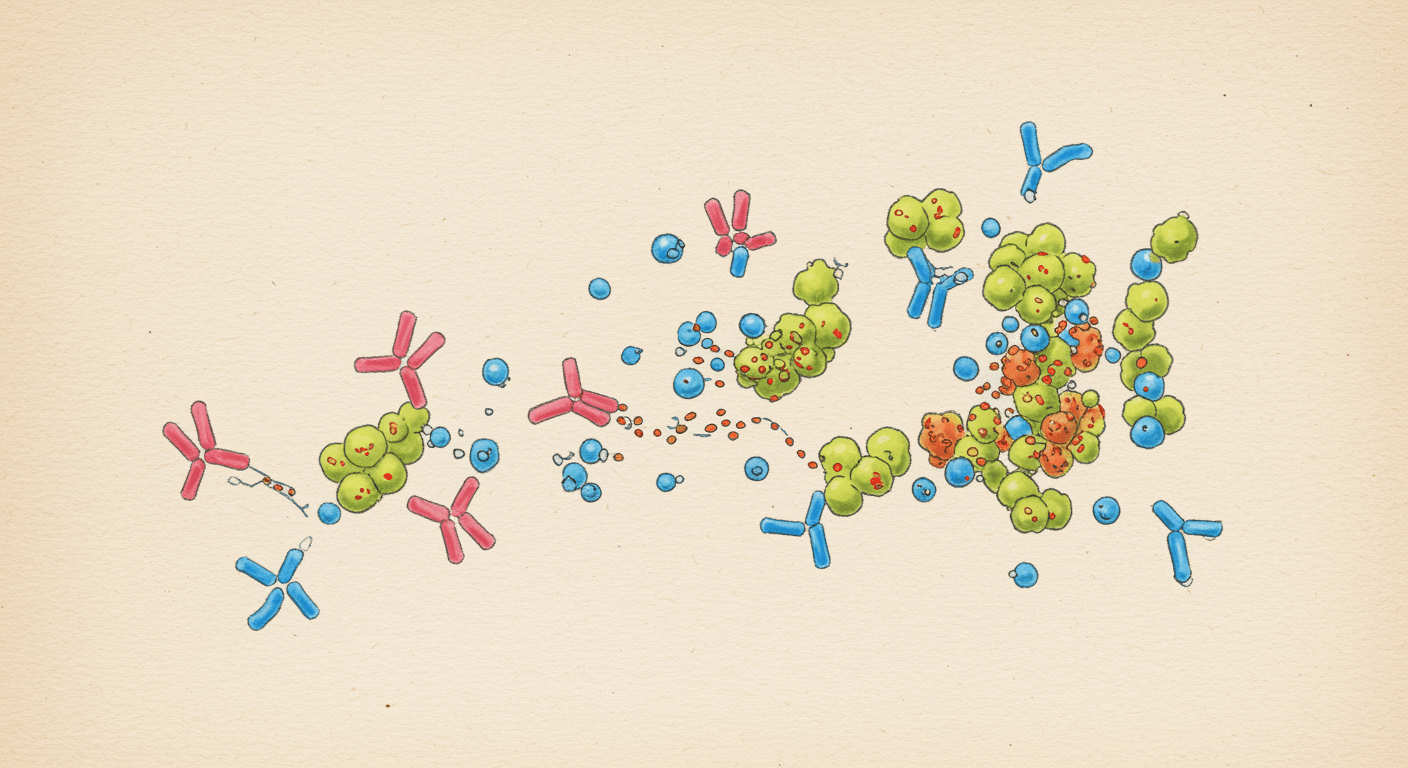
IgG reactions are delayed and inflammatory. When food proteins cross the gut barrier, IgG antibodies bind to them, forming immune complexes. If this exposure is repeated and clearance mechanisms are overwhelmed, these complexes circulate and deposit in tissues, triggering inflammation.
This process explains why food sensitivity symptoms are chronic, multisystemic, and difficult to self-identify.
Secretory IgA is the gut’s first line of immune defence. It binds food antigens in the intestinal lumen, preventing them from crossing into the bloodstream. Chronic stress, infections, and poor nutrition reduce IgA levels, allowing immune exposure to increase.
Low IgA does not cause symptoms directly, but it sets the stage for food sensitivities to develop.
The gut barrier and intestinal permeability
The intestinal lining is only one cell thick. Tight junction proteins regulate what passes through this barrier. When functioning properly, they allow nutrients to pass while blocking large antigenic molecules.
Intestinal permeability occurs when these tight junctions loosen or degrade. Common contributors include:
- Dysbiosis and bacterial overgrowth
- Chronic psychological stress
- Frequent NSAID or antibiotic use
- Gluten exposure in susceptible individuals
- Alcohol and highly processed foods
Once permeability develops, partially digested food proteins enter the bloodstream. The immune system responds by producing antibodies, and food tolerance is lost.
This creates a self-perpetuating cycle where inflammation worsens permeability, and permeability increases immune activation.
Why Indian diets trigger symptoms in vulnerable guts
Dals and legumes contain lectins, saponins, and fermentable carbohydrates. In a healthy gut, these are tolerated. In a sensitive gut, they increase permeability and fermentation, leading to pain and bloating.
Non-celiac gluten sensitivity is common. Gluten and related proteins can activate innate immune pathways and zonulin release, increasing gut permeability even in individuals without celiac disease.
Lactose intolerance is widespread in South India. Additionally, A1 beta-casein found in most commercial milk can produce inflammatory peptides during digestion. Ghee is usually tolerated because milk proteins are removed during clarification.
These are high in fructans and are among the most common triggers for bloating in IBS and SIBO patients.
While many spices are anti-inflammatory, chilli powder and packaged masalas can irritate the gut lining or introduce hidden gluten and additives.
Conditions that mimic food sensitivities
Before concluding that food sensitivities are the primary driver, overlapping conditions must be considered.
Small intestinal bacterial overgrowth
SIBO causes early fermentation of carbohydrates, leading to bloating within 30 to 60 minutes of eating. It also damages the brush border, creating secondary lactose and histamine intolerance.
Parasitic infections
Organisms such as Giardia or Blastocystis can cause chronic symptoms that resemble food reactions.
Fungal overgrowth
Candida and other yeasts can increase permeability and immune activation, contributing to sensitivity patterns.
Addressing these conditions often reduces food sensitivity symptoms significantly.
Diagnostic approach beyond routine testing
Standard allergy tests identify IgE reactions only. They do not detect delayed immune responses.
A functional assessment may include:
- Food-specific IgG or IgA testing as a guide
- Stool analysis to assess IgA levels, inflammation, and pathogens
- Breath testing to evaluate SIBO
However, the most reliable clinical tool remains a structured elimination and reintroduction diet.
The elimination diet as a diagnostic and therapeutic tool
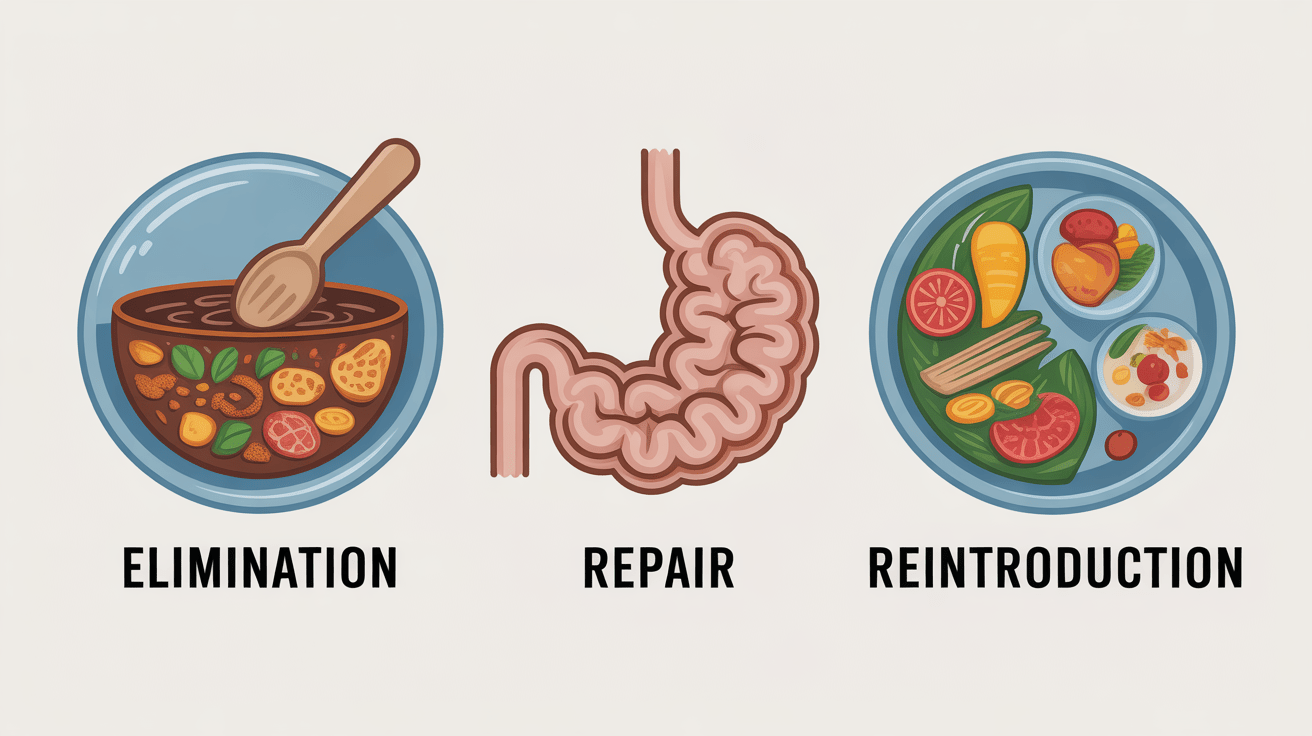
An elimination diet reduces immune load and allows the gut lining to begin healing. It also helps identify trigger foods through systematic reintroduction.
Elimination phase
Typically lasts 3 to 4 weeks. Common triggers such as wheat, dairy, high-FODMAP foods, processed oils, and irritant spices are removed. The diet focuses on well-cooked, low-reactivity foods adapted to Indian cuisine.
Repair phase
Gut-supportive nutrients such as L-glutamine, zinc carnosine, and healthy fats help restore barrier integrity.
Reintroduction phase
Foods are reintroduced one at a time, with a 3-day observation window. Symptoms during this period provide clear evidence of sensitivity.
This process restores clarity and often expands dietary tolerance over time.
Lifestyle factors that determine long-term success
Food alone is not the root cause. Host factors matter.
Stress suppresses digestion and IgA production. Poor sleep impairs gut repair. Eating in a rushed state reduces enzyme output. These factors must be addressed alongside dietary changes to prevent recurrence.
How care is approached at ARKA Anugraha Hospital
At ARKA Anugraha Hospital, food sensitivities are evaluated as part of a broader gut-immune assessment rather than in isolation. Clinical history, dietary patterns, microbial health, and immune markers are considered together.
Under the guidance of Dr Gaurang Ramesh, treatment focuses on restoring tolerance by healing the gut barrier, correcting dysbiosis, and reducing immune overload. The goal is not lifelong restriction, but physiological resilience.
Conclusion
Food sensitivity symptoms are not imagined, exaggerated, or purely functional. They reflect a loss of immune tolerance driven by gut barrier dysfunction and chronic inflammation. In India, where dietary patterns are complex and deeply cultural, recognising this connection is essential.
By identifying triggers, repairing the gut, and supporting immune balance, many patients experience meaningful relief from IBS-like symptoms. Healing is a process, but it is achievable with the right framework.
Frequently Asked Questions
Can food sensitivities cause IBS-like symptoms?
Yes. Many IBS symptoms are driven by delayed immune reactions to food proteins.
Why do symptoms appear hours or days later?
IgG reactions are delayed, unlike immediate IgE allergies.
Are food sensitivities permanent?
Often no. Many resolve once gut health is restored.
Is wheat intolerance always celiac disease?
No. Non-celiac gluten sensitivity is common.
Why do lentils cause bloating in IBS?
They contain fermentable carbohydrates and lectins that irritate sensitive guts.
Can stress worsen food sensitivity symptoms?
Yes. Stress reduces IgA and impairs digestion.
Is ghee safe if I am dairy sensitive?
Usually yes, as it lacks milk proteins and lactose.
Should I avoid all spices?
No. Only irritant or commercial blends may be problematic.
How long does an elimination diet last?
Typically 3 to 4 weeks, followed by reintroduction.
Do I need food sensitivity testing?
Testing can guide elimination but should not replace clinical evaluation.
Can SIBO cause food sensitivities?
Yes. Treating SIBO often improves tolerance.
Why do symptoms affect skin and joints?
Immune complexes circulate and trigger systemic inflammation.
Are children affected by food sensitivities?
Yes, especially after infections or antibiotic exposure.
Can probiotics help?
The right strains at the right time can be beneficial.
Will I ever eat normally again?
Most patients regain dietary flexibility with proper treatment.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
