Prolotherapy for Knee Ligament Injuries: Strengthening Your Joint to Avoid Surgery

- Published on: 28/Jan/2026
- Posted By: Arka Health

Rajesh’s knee instability started after a cricket match at age 42. The software engineer from Bangalore felt his right knee buckle while pivoting to catch a ball. Initially dismissing it as a minor sprain, he noticed his knee continued feeling loose and unreliable. Within months, the instability progressed to constant worry. Climbing stairs required gripping the railing. His knee gave way unexpectedly during normal walking. The deep aching kept him awake at night.
His MRI showed a high grade partial ACL tear with moderate ligament laxity. His orthopedist’s recommendation was clear: ACL reconstruction surgery. The procedure would require harvesting tissue from his hamstring or patellar tendon, months of rehabilitation, and six to nine months before returning to sports. At 42 with demanding work and family responsibilities, Rajesh dreaded the extensive recovery.
When Rajesh discovered prolotherapy at ARKA Anugraha Hospital, he learned something transformative: many knee ligament injuries do not require surgery because the tissue is often mechanically intact but functionally loose. His ACL was stretched and elongated, creating instability without a complete tear requiring grafting. His knee felt unstable not because tissue was missing but because ligament laxity allowed excessive motion grinding his cartilage.
After five prolotherapy sessions over six months, Rajesh’s transformation was remarkable. The buckling sensation vanished. He could pivot confidently, climb stairs normally, and return to recreational cricket. His knee felt stable and strong. Three years later, he remains fully active having avoided surgery through genuine ligament repair and tightening.

Why Your Knee Feels Unstable Even When Your MRI Looks Normal
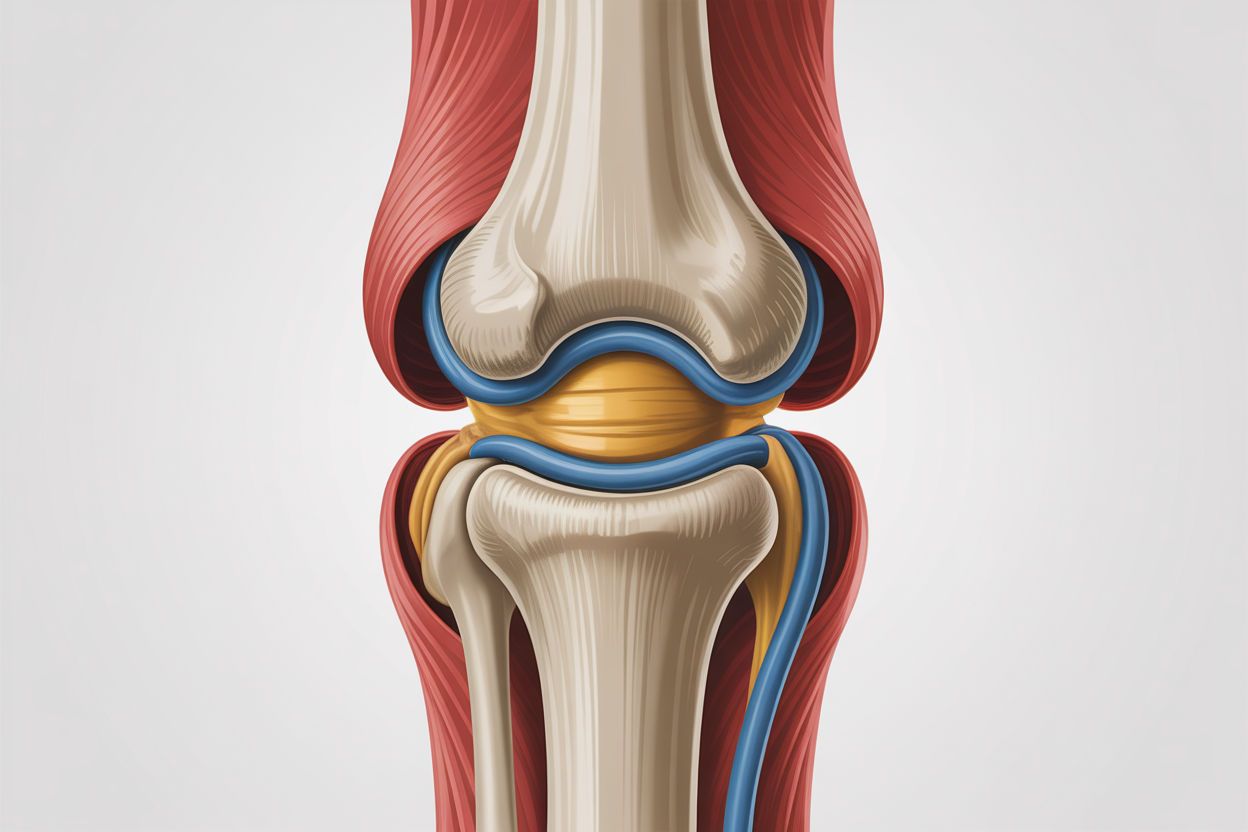
Understanding why prolotherapy succeeds for knee ligament injuries requires recognizing a phenomenon conventional medicine often misses: ligament creep. Your knee’s four primary ligaments including the ACL, PCL, MCL, and LCL provide static stability preventing excessive motion. These ligaments are viscoelastic materials exhibiting both viscous fluid like and elastic solid like properties.
When subjected to constant load over time through poor posture, repetitive athletic trauma, or obesity, ligaments undergo time dependent deformation called creep. Unlike elastic deformation reversing immediately when load removes, creep leads to plastic deformation. Collagen fibers elongate and fail to return to original length. This results in a lax ligament that is mechanically intact with no tear visible on MRI but functionally incompetent.
The joint becomes loose allowing micro movements that shear your articular cartilage. This explains the common frustrating complaint: my knee feels unstable but my doctor says the MRI is normal. Static imaging taken while lying down often misses functional instability, the laxity appearing only when you stand or move under load.
Your ligaments are not inert cables but sophisticated sensory organs densely populated with mechanoreceptors providing proprioceptive feedback telling your brain exactly where your knee is in space. When a ligament stretches or injures, this sensory feedback disrupts. The ligamento muscular reflex, a protective mechanism where muscles surrounding your joint contract to stabilize it when ligaments fail, creates chronic compensatory muscle tightness.
Patients with ligament laxity often present with chronic hamstring or quadriceps tightness. This is not a muscle problem to stretch away but your body’s desperate attempt to stabilize a loose joint. Stretching these muscles without addressing underlying ligament laxity removes the secondary stabilizer, often worsening instability.
Related service: Comprehensive functional knee assessment at ARKA Anugraha Hospital identifies ligament laxity through stress testing and palpation, detecting instability invisible on static MRI.
The Vicious Cycle From Ligament Laxity to Osteoarthritis
Once your knee ligaments become lax, your joint enters a destructive inevitable cascade. There is a direct causal link between ligament laxity and osteoarthritis development. This is not correlation but mechanical inevitability.
Initial injury through micro tear or sprain causes ligament elongation creating laxity. Altered biomechanics follow as joint surfaces no longer glide smoothly but crash and shear. This abnormal motion wears down articular cartilage and meniscus through forces cartilage is not designed to handle. Cartilage brilliantly handles compression but fails under shear grinding stress.
Your body’s defensive response attempts stabilizing the unstable joint by growing extra bone at margins. These osteophytes or bone spurs are not the disease itself but your body’s desperate attempt to widen joint surface and stop instability. The combination of cartilage loss, bone spurs, and chronic pain gets diagnosed as osteoarthritis, but the OA is consequence not cause.
Traditional treatments focusing solely on cartilage through gel injections or pain through NSAIDs fail because they ignore the instability driving destruction. Anti inflammatory medications suppress inflammation but healing requires inflammation. Your body’s natural repair process is an inflammatory cascade. By blocking this, NSAIDs actually inhibit collagen synthesis and ligament repair.
Corticosteroid injections compound the problem being catabolic tissue breaking agents. They inhibit fibroblast activity, weaken collagen, and studies show can accelerate cartilage degeneration. The immediate relief masks progressive structural weakening, creating diminishing returns with each injection.
Read next: Understanding the biomechanical cascade from ligament injury to osteoarthritis at ARKA Anugraha Hospital.
How Prolotherapy Rebuilds Knee Ligament Strength

Prolotherapy succeeds for knee ligament injuries by triggering your body’s own inflammatory pathways to resolve structural deficits conventional treatments ignore. The treatment introduces hypertonic dextrose, typically 12.5 to 25 percent concentration, into the fibro osseous junction where ligament attaches to bone, stimulating a controlled acute healing cascade.
The induction phase spans days one through five. When hypertonic dextrose is injected into extracellular space of your ligament, the high osmolarity causes rapid cellular dehydration and osmotic shock to local cells. This controlled stress causes rupture of a small number of cells releasing intracellular contents, mimicking new injury and tricking your body into reacting. Granulocytes and macrophages recruit to the site releasing potent growth factors including platelet derived growth factor attracting fibroblasts, transforming growth factor beta critical for collagen synthesis, and epidermal growth factor stimulating cell proliferation.
The proliferative phase follows over weeks two through six. Driven by growth factors, fibroblasts migrate to the injection site and begin proliferating rapidly. These construction worker cells synthesize new extracellular matrix, primarily Type III collagen, immature reticular collagen later converted to Type I collagen with high tensile strength. Crucially, prolotherapy stimulates neovascularization, forming new blood vessels. This addresses fundamental hypovascularity of ligaments, bringing permanent increased blood supply to previously oxygen starved injured tissue.
The remodeling phase extends months two through twelve. Initially disorganized new collagen becomes aligned over subsequent months as mechanical load from walking and rehabilitation exercises signals collagen fibers to organize along vectors of stress. The fibers become thicker, denser, and shorter. As collagen matures, it contracts physically tightening the ligament and restoring tension required for joint stability. This phase can continue up to a year, meaning patients often see continued improvement long after injection series completes.
Beyond structural repair, hypertonic dextrose has immediate analgesic effects. It can block TRPV1 receptors involved in pain sensation and hyperpolarize nerve fibers reducing neurogenic inflammation. This provides pain relief distinct from the healing process.
Why Prolotherapy Succeeds Where ACL Surgery Often Falls Short
The decision to operate is irreversible. Once tissue is cut or removed, your knee’s biomechanics permanently alter. While ACL reconstruction is standard and often successful, it carries significant downsides conventional medicine downplays.
Proprioceptive loss represents a hidden cost. Your native ACL is filled with nerve endings providing critical sensory feedback. A graft taken from hamstring or patellar tendon is mechanically functional but sensorially deaf tissue. It provides restraint but lacks the proprioceptive feedback loop essential for coordinated movement. This can lead to altered gait mechanics and future injury risk.
The graft donor site suffers from chronic morbidity including pain and weakness. Athletes who undergo ACL reconstruction using patellar tendon grafts frequently develop chronic anterior knee pain. Hamstring grafts leave the posterior thigh permanently weakened affecting running mechanics.
Paradoxically, stabilizing your knee surgically does not always prevent osteoarthritis. The surgical trauma itself combined with altered kinematics of a graft can lead to early onset OA. Studies show increased arthritis rates in ACL reconstructed knees compared to non surgical management of partial tears in appropriately selected patients.
Prolotherapy offers distinct advantages. It preserves native tissue including critical mechanoreceptors maintaining natural proprioception. The safety profile limits risks to injection related events like temporary bruising or soreness. There is no risk of graft rejection, deep vein thrombosis from immobilization, or surgical infection. Unlike surgery becoming more difficult with each revision, prolotherapy can be repeated as needed to maintain stability if reinjury occurs.
Clinical data supports prolotherapy efficacy. Studies of patients with unresolved knee pain show over 82 percent reporting improvements in walking ability, anxiety, and depression. One study noted 90 percent of patients told surgery was their only option achieved greater than 75 percent pain relief with prolotherapy and avoided operation. In a study covering 1,827 patients, 99 percent found some relief with 75.5 percent reporting complete recovery or cure.
The ARKA Integrative Knee Ligament Protocol

At ARKA Anugraha Hospital, prolotherapy is embedded within comprehensive care recognizing knee health reflects whole body metabolic status. Under Dr. Gaurang Ramesh’s functional medicine guidance, the approach addresses systemic factors that predispose patients to ligament failure and impaired healing.
Metabolic syndrome silently kills connective tissue. Advanced glycation end products form when chronically high blood sugar causes glucose molecules to attach to collagen proteins through glycation. These AGEs act like superglue in wrong places, cross linking collagen fibers indiscriminately. This makes ligaments stiff, brittle, and prone to micro tearing. High glucose levels impair fibroblast function. They migrate slower and produce less collagen. A diabetic patient receiving prolotherapy may have blunted proliferative response compared to metabolically healthy patients.
The gut joint axis dictates inflammation levels in your knees. If gut lining is compromised through leaky gut, bacterial endotoxins leak into bloodstream causing metabolic endotoxemia, systemic low grade inflammation. This systemic inflammation confuses your immune system. When prolotherapy induces local inflammation to signal repair, systemic noise from gut can drown out the signal leading to poor outcomes. Specific gut bacteria produce short chain fatty acids like butyrate critical for regulating immune response and supporting tissue anabolism.
Nutritional biochemistry provides raw materials for ligament regeneration. You cannot build a house without bricks. To synthesize collagen, your body requires specific nutrients. Protein provides glycine, proline, and lysine, the primary structure of collagen triple helix. Vitamin C is essential cofactor for prolyl hydroxylase enzyme stabilizing collagen molecules. Without adequate vitamin C, collagen is weak and falls apart. Zinc is critical for DNA synthesis and cell division; fibroblasts cannot proliferate without adequate zinc. Copper is required for lysyl oxidase enzyme creating cross links giving collagen tensile strength. Omega 3 fatty acids modulate inflammation helping tissue transition from inflammatory to resolution remodeling phase.
Research indicates nutrient timing matters. Consuming vitamin C and collagen gelatin 30 to 60 minutes before physical therapy or loading exercises can double collagen synthesis rate in targeted tissue. This utilizes the pump effect of exercise driving nutrient rich blood into avascular ligaments.
Rehabilitation through progressive loading aligns new collagen along stress vectors. Initial isometric exercises activate muscles without stressing joints. As healing progresses, graduated loading stimulates collagen organization maximizing tensile strength. Biomechanical correction addresses flat feet or weak glutes that caused initial knee stress preventing recurrence.
For patients like Rajesh whose story opened this article, ARKA’s integrative approach provided what surgery oriented care could not: genuine ligament tightening and stabilization through stimulating his body’s innate regenerative capacity while optimizing the metabolic terrain enabling that healing.
Your knee ligament injury does not have to mean accepting instability or facing invasive surgery. When conventional treatments fail to address ligament laxity and the systemic factors preventing healing, prolotherapy offers evidence based hope for preserving your native knee structures and restoring stable pain free function.
FREQUENTLY ASKED QUESTIONS
- What is ligament creep and how does it cause knee instability? Ligament creep describes time dependent deformation where ligaments subjected to constant load through poor posture, repetitive trauma, or obesity undergo plastic deformation. Unlike elastic deformation that reverses when load removes, creep causes collagen fibers to elongate permanently and fail to return to original length. This creates a lax ligament that is mechanically intact without visible MRI tear but functionally incompetent. The loose ligament allows excessive joint motion creating micro instability where your femoral and tibial surfaces crash and shear rather than gliding smoothly. This explains why your knee feels unstable but imaging appears normal. Prolotherapy specifically tightens these crept ligaments by stimulating new collagen synthesis that contracts and shortens the elongated tissue restoring proper tension.
- Can prolotherapy help partial ACL tears without requiring surgery? Yes, prolotherapy offers significant hope for partial ACL tears and non retracted complete tears. The dogma that ACLs cannot heal is being challenged by regenerative medicine. Recent case studies document successful non surgical repair of high grade partial and even complete ACL tears using prolotherapy. The mechanism involves intra articular prolotherapy injections bathing the ACL in growth factors. While synovial fluid usually washes away healing clots, repeated proliferant introduction every four to six weeks maintains a healing environment overcoming hostile joint physiology. Post treatment MRIs in documented cases show restored continuity of ligament fibers previously disrupted. This approach is ideal for non professional athletes not requiring immediate sport return or patients wishing to avoid lengthy rehabilitation and proprioceptive loss associated with surgical grafts.
- Why do anti inflammatory medications prevent my knee ligaments from healing? Anti inflammatory medications including NSAIDs like ibuprofen and diclofenac block cyclooxygenase enzymes reducing prostaglandin production. While this suppresses pain signals, it simultaneously stops healing signals because prostaglandins are essential mediators of tissue repair. Your body’s natural repair process requires acute controlled inflammation as the prerequisite for healing. Inflammatory cascades recruit growth factors and fibroblasts needed for collagen synthesis. By blocking inflammation, NSAIDs actually inhibit ligament repair and collagen production. Studies confirm NSAIDs can slow or arrest connective tissue healing. This is why prolotherapy protocols strictly prohibit NSAID use for one week before and two weeks after treatment, allowing the deliberately induced healing inflammation to complete its regenerative work.
- How does prolotherapy compare to PRP or stem cell therapy for knee ligaments? Prolotherapy using hypertonic dextrose is the foundational regenerative treatment acting as a signal recruiting your body’s existing stem cells and growth factors to migrate to injured areas. It is highly effective and cost efficient for most knee ligament laxity. PRP platelet rich plasma involves concentrating your blood platelets delivering higher growth factor doses directly, useful for more severe degeneration or cases where dextrose response is insufficient. Stem cell therapy involves harvesting and injecting regenerative cells reserved for significant tissue loss. At ARKA, treatment typically begins with dextrose prolotherapy due to excellent efficacy and value. PRP or stem cells are considered for more severe cases, often used synergistically. Prolotherapy’s advantage is standardized effectiveness regardless of patient age or blood quality unlike PRP dependent on platelet function.
- Why does my knee hurt more immediately after prolotherapy injection? The increased pain represents the induction phase where prolotherapy intentionally creates controlled inflammation. The hypertonic dextrose causes osmotic cellular stress releasing inflammatory mediators that recruit immune cells and growth factors. This mimics acute injury tricking your body into initiating repair. Pain typically peaks at 24 to 48 hours then subsides as the inflammatory phase transitions to proliferation. This temporary soreness is actually a positive sign indicating your immune system is responding vigorously to treatment. If you felt nothing, it might mean inadequate response. The healing pain differs qualitatively from your chronic instability pain, described as deep ache or soreness rather than sharp instability. This confirms the regenerative cascade has successfully initiated.
- Can prolotherapy help if I already had meniscus surgery but still have pain? Yes, prolotherapy is highly recommended after meniscectomy. Meniscus removal creates instability because the spacer is gone putting more stress on ligaments and cartilage. This explains why many patients develop progressive pain and arthritis after meniscus surgery despite technically successful procedures. Prolotherapy tightens surrounding ligaments including the coronary ligaments anchoring meniscus remnants to tibia, compensating for missing meniscus tissue. By restoring capsular tension and ligament stability, prolotherapy stabilizes your joint and slows osteoarthritis progression. Many post meniscectomy patients who were told arthritis is inevitable find substantial relief and functional improvement through ligament strengthening even though meniscus cannot regenerate.
- How does metabolic syndrome affect my knee ligament healing capacity? Metabolic syndrome profoundly impairs connective tissue healing through multiple mechanisms. Chronically elevated blood sugar causes glucose molecules to bind collagen proteins forming advanced glycation end products that cross link collagen fibers indiscriminately making them brittle and prone to tearing. High glucose impairs fibroblast function causing them to migrate slower and produce less collagen, blunting proliferative response to prolotherapy. Insulin resistance creates systemic inflammation that confuses immune signaling needed for coordinated healing. Adipose tissue releases pro inflammatory adipokines creating biochemical assault on joints beyond mechanical weight burden. At ARKA Anugraha Hospital, all knee pain patients receive HbA1c screening and metabolic optimization because prolotherapy works most effectively when the biological terrain supports healing.
- What makes ARKA’s prolotherapy protocol different from standalone injection clinics? ARKA Anugraha Hospital practices integrative orthopedics recognizing injection therapy represents only 50 percent of healing equation. Under Dr. Gaurang Ramesh’s functional medicine leadership, the comprehensive approach addresses systemic factors determining healing capacity. This includes gut health screening treating leaky gut that causes systemic inflammation blunting prolotherapy signals, metabolic optimization correcting insulin resistance and glycation that impairs fibroblast function, nutritional biochemistry providing raw materials like vitamin C, zinc, and collagen for tissue synthesis, and biomechanical rehabilitation correcting movement patterns that caused initial injury. This total patient approach optimizing the biological terrain ensures prolotherapy injections produce maximal structural repair rather than just providing temporary symptom relief.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
