Vagus Nerve Dysfunction and Digestive Problems: How ARKA Anugraha Hospital Restores Gut-Brain Health
- Published on: 18/Dec/2025
- Posted By: Arka Health

Many people living with chronic digestive problems are told they have IBS, acidity, reflux, or functional dyspepsia. They may try antacids, laxatives, probiotics, or repeated antibiotic courses, yet their symptoms return again and again. Bloating persists even on small meals. Constipation alternates with loose stools. Acid reflux flares during stress. Nausea appears without warning.
What often goes unrecognised is that digestion is not controlled by the gut alone. It is directed by the nervous system, particularly a powerful nerve called the vagus nerve. When this nerve loses its tone or signalling capacity, digestion loses rhythm, coordination, and resilience. This state is known as vagus nerve dysfunction.
At ARKA Anugraha Hospital in Bengaluru, vagus nerve dysfunction is recognised as a central driver behind many chronic digestive disorders. Under the care of Dr Gaurang Ramesh, treatment focuses not only on suppressing symptoms but on restoring gut-brain communication through integrative gastroenterology, functional diagnostics, and targeted neuromodulation therapies.
This article explains how vagus nerve dysfunction affects digestion, why symptoms become chronic, and how ARKA Anugraha Hospital approaches treatment in a structured and evidence-based manner.
1. Understanding the Vagus Nerve and Its Role in Digestion
The vagus nerve is the tenth cranial nerve and the primary parasympathetic nerve of the body. It originates in the brainstem and travels down the neck into the chest and abdomen, supplying the heart, lungs, liver, pancreas, stomach, and intestines.
It is often described as the main nerve of the rest and digest system.
When the vagus nerve is functioning well, it:
- Slows the heart rate
- Reduces inflammation
- Stimulates stomach acid and enzyme secretion
- Coordinates intestinal motility
- Activates the migrating motor complex
- Supports gut barrier integrity
In modern lifestyles dominated by chronic stress, irregular meals, infections, and metabolic strain, vagal activity is frequently suppressed. The nerve remains anatomically intact but functionally underactive. This creates a state of autonomic imbalance where the stress response dominates and digestion is compromised.
2. The Gut-Brain Axis and Why Digestion Depends on Neural Tone
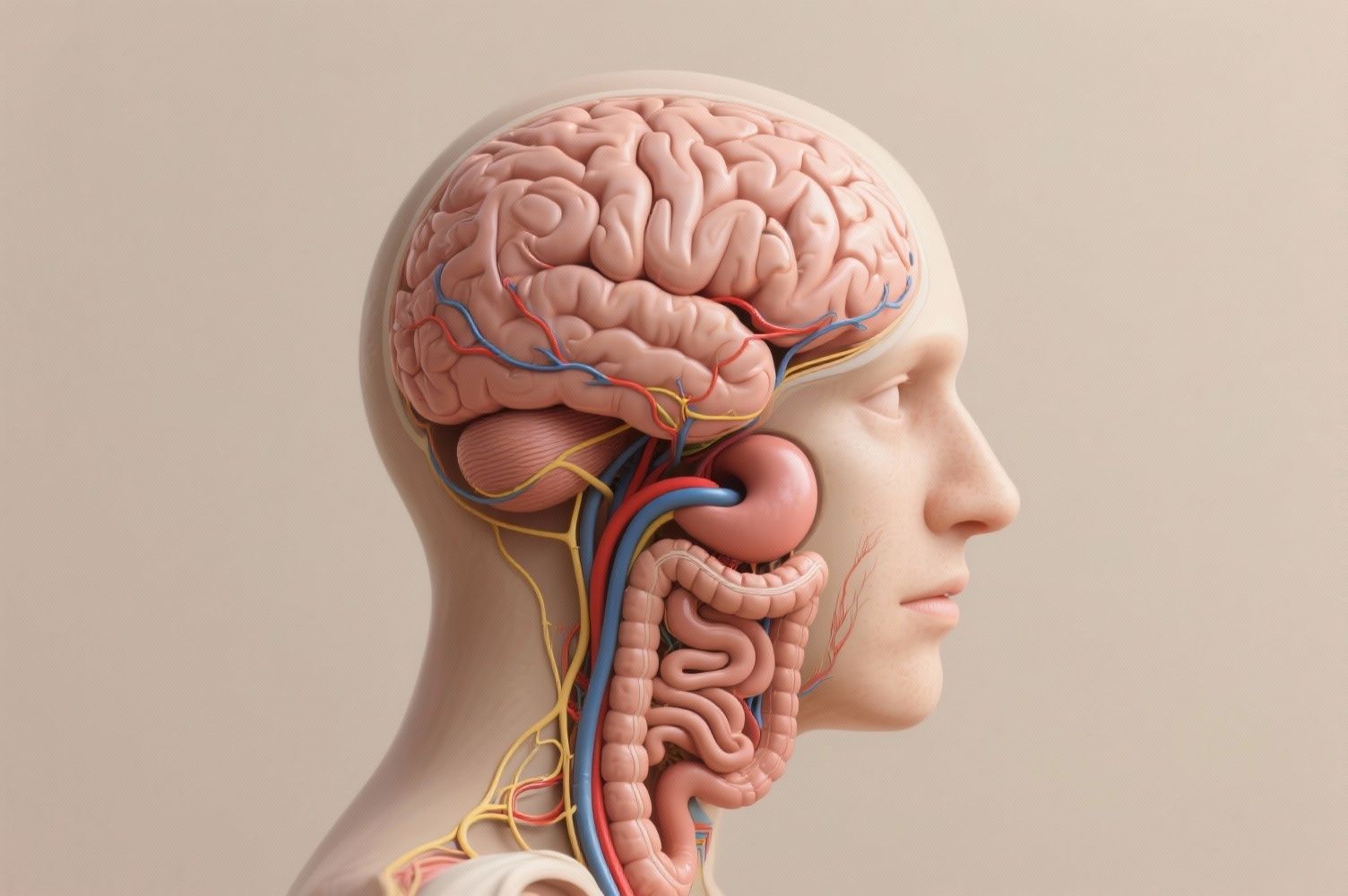
The gut-brain axis refers to the continuous two-way communication between the digestive tract and the central nervous system. The vagus nerve is the main communication highway within this system.
Importantly, most vagal fibres are sensory. Around eighty percent of signals travel from the gut to the brain. These signals inform the brain about stretch, nutrient content, inflammation, and microbial activity. Only a smaller portion of fibres send commands from the brain to the gut.
When vagal signalling is impaired:
- The brain receives distorted information from the gut
- Satiety signals are blunted or exaggerated
- Inflammatory signals remain unchecked
- Pain perception increases
- Motility patterns become disorganised
This explains why anxiety worsens gut symptoms and why gut inflammation worsens mood. The relationship is biological, not psychological.
3. What Causes Vagus Nerve Dysfunction
Prolonged stress keeps the nervous system locked in sympathetic dominance. Over time, parasympathetic activity declines, leading to low vagal tone. Emotional trauma can also trigger protective shutdown patterns that suppress digestion.
Viruses such as Epstein Barr, influenza, and SARS-CoV-2 can inflame neural tissue. Many patients develop new digestive symptoms after viral illness, including gastroparesis and IBS-like patterns.
Diabetes is a well-known cause of autonomic neuropathy. High glucose damages the small blood vessels that nourish the vagus nerve, impairing signal transmission.
Endotoxins released by harmful bacteria blunt vagal sensory receptors. This disrupts satiety signalling and inflammatory feedback loops.
The vagus nerve passes through the neck alongside major blood vessels. Poor posture, chronic device use, and cervical instability can mechanically irritate the nerve and alter its function.
4. Digestive Symptoms Linked to Vagus Nerve Dysfunction

Because the vagus nerve supplies multiple organs, symptoms often span different systems.
Digestive symptoms
- Chronic bloating
- Early fullness
- Nausea
- Acid reflux
- Alternating constipation and diarrhoea
- Difficulty swallowing
- Abdominal pain
Systemic symptoms
- Anxiety and low mood
- Brain fog
- Palpitations
- Dizziness on standing
- Fatigue
Many patients undergo extensive testing without clear findings because standard investigations do not assess neural function.
5. How Vagus Nerve Dysfunction Disrupts Digestion
The vagus nerve controls stomach contractions. When its signalling is reduced, food stagnates in the stomach, leading to nausea, bloating, and vomiting.
The migrating motor complex is a cleaning wave that sweeps bacteria and debris from the small intestine between meals. Low vagal tone disables this mechanism, allowing bacterial overgrowth.
SIBO is closely linked to vagus nerve dysfunction. Without proper motility and ileocecal valve control, bacteria migrate into the small intestine and ferment food, producing gas and inflammation.
The vagus nerve initiates the cephalic phase of digestion. Reduced signalling leads to hypochlorhydria and pancreatic enzyme insufficiency, worsening maldigestion and nutrient deficiencies.
Vagal signalling supports tight junction proteins that maintain gut barrier integrity. When tone is low, intestinal permeability increases, allowing toxins and food antigens into circulation.
6. Diagnostic Approach at ARKA Anugraha Hospital

ARKA combines conventional gastroenterology with advanced functional diagnostics.
Endoscopy and imaging
Used to exclude ulcers, tumours, and structural disease.
Heart rate variability testing
Heart rate variability is a direct marker of vagal tone. Low variability indicates autonomic rigidity and poor parasympathetic activity. ARKA uses HRV to assess baseline dysfunction and monitor recovery.
Breath testing
Hydrogen and methane breath tests detect SIBO and carbohydrate malabsorption, common downstream effects of vagus nerve dysfunction.
Motility studies
Gastric emptying scans and manometry identify delayed transit and coordination disorders.
Stool and immune markers
These tests assess inflammation, microbial balance, and gut immune activity.
7. Treatment Philosophy at ARKA Anugraha Hospital
8. Ozone Therapy as a Neural and Gut Modulator
Ozone therapy is a key integrative modality at ARKA Anugraha Hospital.
Medical ozone acts as a controlled biological stimulus that:
- Activates antioxidant defence systems
- Improves tissue oxygen delivery
- Modulates immune signalling
- Reduces pathogenic bacterial load
Research shows ozone can shift autonomic balance toward parasympathetic dominance and improve heart rate variability. This makes it particularly valuable in vagus nerve dysfunction.
Ozone is administered through techniques such as rectal insufflation or autohemotherapy, depending on the clinical context.
9. Vagus Nerve Stimulation Therapy
ARKA employs non-invasive vagus nerve stimulation methods.
Auricular vagus nerve stimulation
The vagus nerve has a surface branch in the ear. Gentle electrical stimulation in this area sends signals directly to the brainstem, improving motility, reducing inflammation, and calming pain pathways.
Clinical benefits observed
- Improved gastric emptying
- Reduced nausea and bloating
- Better bowel regularity
- Lower inflammatory markers
- Improved mood and sleep
Vagus nerve stimulation is often combined with breathing exercises to amplify parasympathetic activation.
10. Sound Therapy and Frequency-Based Neuromodulation

Sound therapy is used as a form of physical neuromodulation rather than relaxation alone.
Low-frequency vibrations and auditory entrainment influence autonomic centres in the brainstem. Humming and chanting stimulate vagal branches in the throat and larynx, creating direct mechanical activation.
These therapies help reduce cortisol levels, improve heart rate variability, and ease gut spasm and pain.
11. Acupuncture as Autonomic Regulation
Acupuncture modulates autonomic function through somatic afferent stimulation.
Points such as ST36 and PC6 are used to:
- Improve gastric motility
- Reduce nausea
- Calm visceral hypersensitivity
- Enhance vagal tone
At ARKA, acupuncture is integrated with medical management rather than used in isolation.
12. Nutrition That Supports Vagal Recovery
Diet is approached as neuro-supportive therapy.
Low FODMAP strategies
Used temporarily to reduce fermentation and sensory overload in SIBO.
Anti-inflammatory protocols
Remove foods that perpetuate immune activation and sympathetic dominance.
Targeted prebiotics
Fibres such as PHGG are introduced carefully to support short-chain fatty acid production without triggering symptoms.
Key nutrients
- Choline for acetylcholine synthesis
- Omega-3 fatty acids for neural membranes
- Selected psychobiotic strains that communicate with the brain via the vagus nerve
13. Yoga and Breathwork for Vagus Nerve Health
Active patient participation is essential.
Slow breathing with extended exhalation directly stimulates vagal activity. Diaphragmatic breathing massages the nerve as it passes through the diaphragm.
Yoga postures that compress or gently stretch the abdomen and throat further enhance neural signalling and digestive rhythm.
14. A Typical Patient Journey at ARKA
A patient with long-standing bloating and constipation presents after multiple failed treatments. Breath testing confirms methane-dominant SIBO. Heart rate variability reveals low vagal tone.
Treatment includes:
- Dietary modification
- Ozone therapy
- Auricular vagus nerve stimulation
- Prokinetic support
- Breathwork and yoga
Within weeks, bloating reduces and bowel movements normalise. Over months, autonomic balance improves and relapse risk decreases.
15. Why ARKA Anugraha Hospital Is Different
ARKA bridges the gap between conventional gastroenterology and functional neurology.
- Structural disease is ruled out safely
- Functional drivers are identified precisely
- Neural regulation is treated directly
- Integrative therapies are evidence-informed
- Care is physician-led and medically supervised
Dr Gaurang Ramesh’s dual expertise allows patients to receive both diagnostic safety and deeper healing.
Digestive disorders are rarely isolated gut problems. They are often expressions of nervous system imbalance. Vagus nerve dysfunction disrupts motility, immunity, and perception, creating the chronic patterns seen in IBS, SIBO, reflux, and functional dyspepsia.
At ARKA Anugraha Hospital, treatment focuses on restoring communication between the gut and brain. By addressing neural tone alongside microbial balance and inflammation, patients are offered a sustainable path toward recovery.
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
