Preparing for Pregnancy: Preconception Checklist (Labs + Lifestyle) for ARKA Anugraha Hospital

Published on: 24/Nov/2025
Posted By: Arka Health

The decision to bring a new life into the world is perhaps the most significant biological and emotional undertaking a couple will ever navigate. In the contemporary healthcare landscape, the focus has largely remained on the prenatal period—the nine months of gestation following a positive pregnancy test. However, a paradigm shift is currently underway, spearheaded by forward-thinking institutions like Arka Anugraha Hospital in JP Nagar, Bangalore. This shift recognizes that the health of the future child is fundamentally programmed during the preconception window—the critical 90 to 120 days leading up to fertilization.
This comprehensive research report serves as an exhaustive guide for couples preparing for pregnancy. It integrates the rigorous safety protocols of conventional obstetrics—adhering to guidelines from the Federation of Obstetric and Gynaecological Societies of India (FOGSI) and the American College of Obstetricians and Gynecologists (ACOG)—with the root-cause analysis of Functional Medicine. Functional Medicine, a modality passionately championed by Dr. Gaurang Ramesh at Arka Anugraha, seeks to optimize the biological terrain of the parents to ensure the highest quality genetic material is passed to the offspring.
This document details the specific laboratory investigations required (both standard and advanced), nutritional strategies tailored to the Indian palate and Ayurvedic traditions, environmental detoxification protocols to mitigate endocrine disruption, and the lifestyle modifications necessary to “prime” the body for conception. By bridging the gap between modern surgical excellence—offered by experts like Dr. Ramesh Makam—and holistic internal medicine, Arka Anugraha Hospital offers a unique, integrative pathway to parenthood.
1. The Integrative Paradigm: Redefining Preconception Care
1.1 The Biological Window of Opportunity
To understand why preconception care is vital, one must first understand the biology of gametogenesis—the creation of sperm and egg. Conventional wisdom often assumes that health interventions begin only after a missed period. However, the biological reality is that the genetic material (DNA) and the cellular machinery (mitochondria) of the egg and sperm are developing for months prior to the moment of conception.
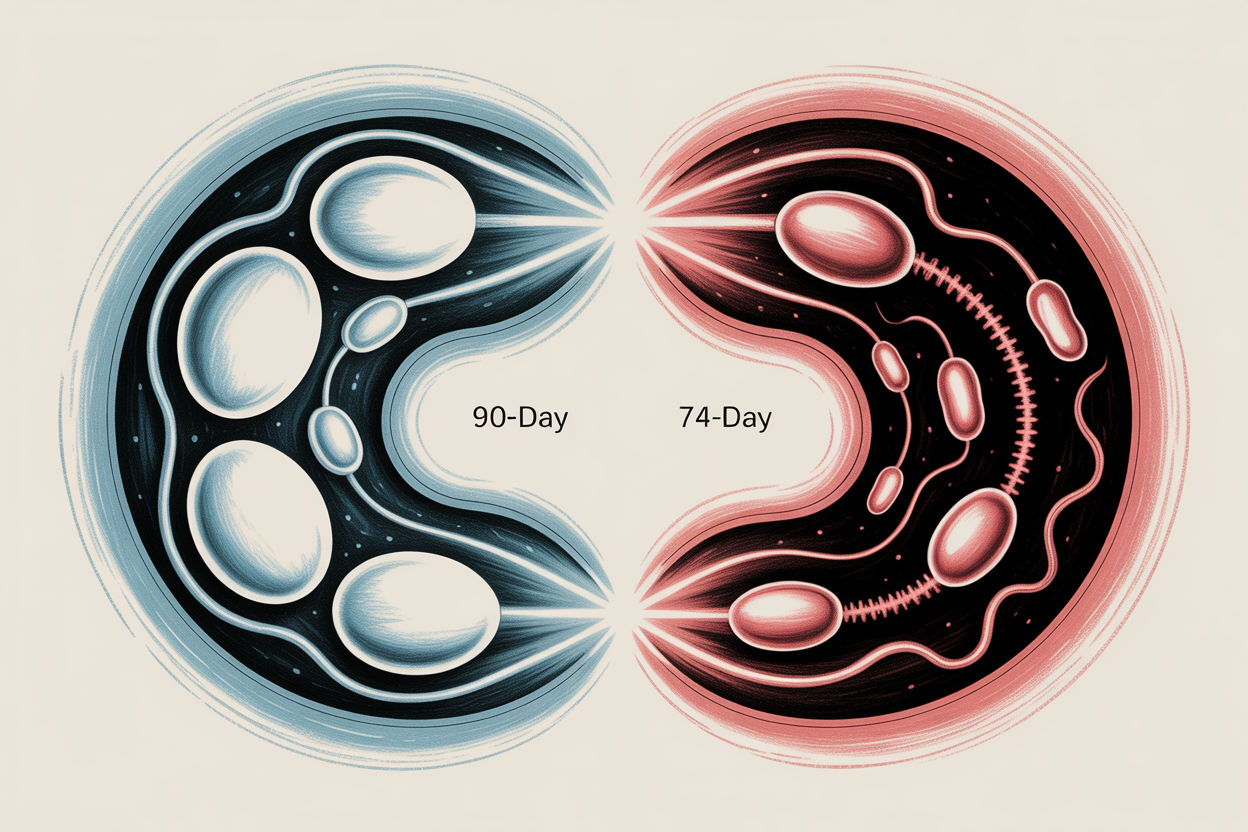
The 90-Day Egg Journey (Folliculogenesis):
While a woman is born with all the eggs she will ever have, these eggs exist in a dormant state. Approximately three to four months before ovulation, a cohort of dormant follicles is recruited to begin the maturation process. During this 90-day window, the egg undergoes rapid metabolic activity and chromosomal division. It is during this phase that the egg is most vulnerable to the internal environment—influenced by nutrient density, hormonal balance, and oxidative stress. If the mother’s body is inflamed or nutrient-depleted, the egg quality suffers, potentially leading to chromosomal abnormalities (aneuploidy) or mitochondrial dysfunction, which are leading causes of early miscarriage.
The 74-Day Sperm Cycle (Spermatogenesis):
Similarly, sperm production is a continuous process that takes approximately 72 to 74 days from germ cell to mature spermatozoa. Unlike the egg, sperm are generated de novo throughout a man’s life. This means that the lifestyle choices a man makes today—what he eats, whether he smokes, his stress levels—will be reflected in the sperm he ejaculates three months from now. This provides a powerful window of opportunity where interventions can dramatically improve sperm count, motility, and morphology.
1.2 The Arka Anugraha Difference: Functional vs. Conventional
Arka Anugraha Hospital distinguishes itself as India’s first NABH Accredited Integrative & Functional Medicine Hospital. This accreditation is not merely a label but a testament to a fundamental difference in philosophy.
In a conventional setting, preconception care is often a screening exercise designed to identify overt pathology. The questions asked are binary: Does the patient have rubella immunity? Is there HIV? Is the fallopian tube blocked? While these are critical safety questions, they do not address optimization.
At Arka Anugraha, the approach integrates Functional Medicine, which views health as a continuum rather than a switch between “healthy” and “diseased.” Under the guidance of Dr. Gaurang Ramesh, an Integrative Gastroenterologist and Functional Medicine practitioner, the clinical team asks deeper questions:
- Conventional: Is the patient’s Thyroid Stimulating Hormone (TSH) within the lab reference range of 0.5 to 5.0 mIU/L?
- Functional: Is the thyroid function optimal for fertility (TSH < 2.5 mIU/L)? Are there subclinical autoimmune antibodies attacking the thyroid gland, even if TSH is normal?.
- Conventional: Is the patient menstruating regularly?
- Functional: Is the patient ovulating robustly? Is there sufficient progesterone to support the luteal phase? Is gut dysbiosis causing the recirculation of toxic estrogens (the estrobolome connection)?.
This integrative model combines the surgical precision of Dr. Ramesh Makam—who brings over 35 years of expertise in bariatric and laparoscopic surgery for conditions like fibroids or obesity-related infertility—with the metabolic detective work of functional medicine.
1.3 The Epigenetic Responsibility
The concept of “fetal programming,” often referred to as the Barker Hypothesis, suggests that the environment in the womb determines the child’s susceptibility to chronic diseases decades later, such as diabetes, hypertension, and heart disease. Functional preconception care extends this timeline back to the pre-pregnancy period. By optimizing parental health before conception, couples are essentially “cleaning the soil” before planting the seed, thereby influencing the epigenetic switches that control the child’s health destiny. This is the core mission of Arka Anugraha’s preconception program: to create a legacy of health.
2. The Medical Foundation: Conventional Laboratory Investigations
Before exploring advanced functional testing, it is imperative to establish a safety baseline. These tests are the non-negotiables—the standard of care recommended by ACOG and FOGSI to rule out infectious diseases, genetic carrier states, and frank organ dysfunction.
2.1 For Her: The Essential Maternal Safety Panel
This panel is designed to identify conditions that could pose immediate risks to the mother or the developing fetus.
2.1.1 Complete Blood Count (CBC) & Hemoglobin Analysis
What it tests: Red blood cells, white blood cells, and platelets.
Why it matters in India: Anemia is a public health crisis in India, with studies indicating extremely high prevalence among women of reproductive age. Hemoglobin levels below 11 g/dL are associated with an increased risk of preterm delivery, low birth weight, and postpartum hemorrhage.
The Insight: If hemoglobin is low, it is crucial to differentiate between Iron Deficiency Anemia (IDA) and Thalassemia Trait. In India, blindly prescribing iron supplements without ruling out Thalassemia can be dangerous, as Thalassemia carriers can suffer from iron overload.
2.1.2 Blood Grouping & Rh Factor
What it tests: A, B, AB, or O blood type and Rhesus (Rh) status (positive or negative).
Why it matters: The primary concern is Rh Incompatibility. If an Rh-negative woman conceives with an Rh-positive partner, the baby may be Rh-positive. During delivery or any event where fetal blood mixes with maternal blood, the mother’s immune system may develop antibodies against the Rh factor (isoimmunization). While the first baby is usually safe, these antibodies can attack the red blood cells of future pregnancies, causing hemolytic disease of the newborn. Knowing Rh status in advance allows for strict monitoring and the administration of Anti-D immunoglobulin prophylaxis.
2.1.3 Rubella (German Measles) IgG Immunity
What it tests: Immunity levels against the Rubella virus.
Why it matters: Rubella is a mild illness for adults but devastating for a developing fetus. Infection during the first trimester can cause Congenital Rubella Syndrome (CRS), leading to deafness, cataracts, and cardiac defects.
The Action Plan: If IgG levels are low (non-immune), the woman must be vaccinated with the MMR vaccine. Since MMR is a live attenuated virus, it is strictly contraindicated during pregnancy. Women are advised to wait at least one month (FOGSI recommendation) or ideally three months after vaccination before attempting to conceive.
2.1.4 Thalassemia Screening (Hb Electrophoresis)
What it tests: Analysis of hemoglobin types to detect carrier status for Beta-Thalassemia.
Why it matters: Thalassemia is a genetic blood disorder prevalent in certain Indian communities. If both parents are carriers (Thalassemia Minor), there is a 25% statistical probability that their child will be born with Thalassemia Major, a condition requiring lifelong blood transfusions. Preconception screening allows couples to make informed reproductive choices.
2.1.5 Infectious Disease Panel (The “TORCH” & More)
- Hepatitis B (HBsAg): Vertical transmission from mother to child is a leading cause of chronic Hepatitis B. Screening ensures that if the mother is positive, the infant can receive immunoglobulin and vaccination immediately after birth.
- HIV & Syphilis (VDRL): Screening is mandatory to prevent transmission. Untreated syphilis can lead to stillbirth.
- Varicella (Chickenpox): Women with no history of chickenpox should be screened for immunity. Varicella pneumonia during pregnancy is a severe complication.
2.1.6 Pap Smear & Pelvic Examination
What it tests: Cervical cell health and structural anatomy.
Why it matters: A Pap smear screens for cervical dysplasia caused by HPV. Treating cervical issues is safer and easier before pregnancy than during. A physical pelvic exam can also identify structural abnormalities like fibroids or ovarian cysts, which might interfere with implantation. Dr. Ramesh Makam’s team at Arka specializes in minimally invasive laparoscopic management of such structural issues if they are identified.
2.2 For Him: The Male Factor Baseline
Infertility is a shared journey, with male factors contributing to approximately 40-50% of cases. It is archaic to investigate only the female partner.
2.2.1 Semen Analysis
What it tests:
- Count: Concentration of sperm per milliliter (World Health Organization cutoff: >15 million/ml).
- Motility: Percentage of sperm that are moving (progressive motility is key).
- Morphology: The shape of the sperm (normal forms >4% by Kruger strict criteria).
The Insight: Sperm parameters are highly volatile and can be affected by recent illness, heat exposure, or stress. A single “poor” result is rarely diagnostic; a repeat test 4-6 weeks later is standard practice.
2.2.2 Infectious Disease Screening
What it tests: HIV, Hepatitis B, Hepatitis C, Syphilis.
Why it matters: Sexual transmission of these infections to the female partner during unprotected intercourse (trying to conceive) poses a risk to both the mother and the future fetus.
3. The Functional Deep Dive: Optimization Labs
Once the safety baseline is established, the Arka Anugraha approach pivots to Functional Medicine. This layer of testing is designed to uncover “root causes”—the subtle biochemical imbalances that may not be classified as “diseases” yet but act as barriers to optimal fertility. This approach is deeply integrated into Dr. Gaurang Ramesh’s practice, utilizing advanced diagnostics to restore balance.
3.1 The Comprehensive Thyroid Panel (Beyond TSH)
The Conventional View: Measure TSH. If it is between 0.5 and 5.0, the thyroid is “normal.”
The Functional View: TSH is a pituitary signal, not a thyroid hormone. A “normal” TSH does not guarantee that the cells are receiving enough energy. For fertility, the thyroid demands are high.
The Panel:
- Free T3 (FT3) & Free T4 (FT4): These are the unbound, active hormones. Low FT3 (the biologically active form) can lead to anovulation or luteal phase defects even if TSH is normal.
- Reverse T3 (rT3): During times of chronic stress, trauma, or extreme dieting, the body converts T4 into Reverse T3 instead of Free T3. rT3 acts as a “brake,” blocking thyroid receptors. High rT3 is a sign of a body in “survival mode”—not a reproductive state.
- Thyroid Antibodies (Anti-TPO & Anti-TG): The presence of these antibodies indicates Hashimoto’s Thyroiditis, an autoimmune condition. Studies suggest that the presence of thyroid antibodies, even with normal thyroid function, is associated with a higher risk of miscarriage and implantation failure. Identifying autoimmunity early allows for dietary interventions (like gluten elimination) to reduce antibody load.
- Optimal Range: For conception, most integrative endocrinologists aim for a TSH between 1.0 and 2.5 mIU/L.
3.2 Metabolic Health & Insulin Resistance
The Conventional View: Fasting glucose < 100 mg/dL is normal.
The Functional View: Glucose is a lagging indicator. Insulin is the leading indicator. Many women, especially those with Polycystic Ovary Syndrome (PCOS), maintain normal blood sugar by pumping out massive amounts of insulin.
The Mechanism: High insulin levels stimulate the ovaries (theca cells) to produce excess androgens (testosterone). This arrests follicular development, leading to irregular cycles and “cysts” on the ovaries.
The Panel:
- Fasting Insulin: Optimal functional range is often < 8 uIU/mL (Standard lab range goes up to 25).
- HbA1c: Average blood sugar over 3 months. Ideally < 5.4% for pregnancy.
- HOMA-IR: A calculation based on glucose and insulin that quantifies insulin resistance.
3.3 The Gut-Fertility Axis (Dr. Gaurang’s Specialty)
Dr. Gaurang Ramesh emphasizes the “5 Rs” of gut health (Remove, Replace, Reinoculate, Repair, Rebalance) because the gastrointestinal tract is the epicenter of systemic inflammation.
The Mechanism:
- The Estrobolome: This is a specific collection of bacteria in the gut responsible for metabolizing and eliminating used estrogen. If the gut microbiome is imbalanced (dysbiosis) or if there is constipation, beta-glucuronidase enzymes can “unpack” the estrogen packaged for disposal, allowing it to be reabsorbed into the bloodstream. This leads to “Estrogen Dominance,” a driver of conditions like endometriosis, fibroids, and heavy periods.
- Nutrient Absorption: You are not what you eat; you are what you absorb. A damaged gut lining (Leaky Gut) impairs the absorption of Zinc, Iron, and B12—all critical for fertility.
- Systemic Inflammation: When the gut barrier is compromised, toxins (LPS) leak into the blood, triggering an immune response. The body perceives this chronic inflammation as an unsafe environment for pregnancy, potentially hindering implantation.
The Panel:
- Comprehensive Stool Analysis (GI-MAP): Tests for commensal bacterial balance, pathogens, parasites, and markers of inflammation (Calprotectin).
- Food Sensitivity Testing: Identifies specific triggers (like gluten or dairy) that may be causing low-grade inflammation.
3.4 Vitamin D & Nutrient Status
Vitamin D (25-OH): It is actually a pro-hormone, not a vitamin. It is essential for the production of sex hormones and the regulation of the immune system (preventing the rejection of the embryo).
- Prevalence: Despite ample sunlight, Vitamin D deficiency is rampant in India due to skin pigmentation and indoor lifestyles.
- Optimal Range: Functional medicine aims for 50–70 ng/mL for fertility, whereas < 20 ng/mL is considered deficient.
Iron & Ferritin: Ferritin is the storage form of iron. Low ferritin (< 30 ng/mL) is a common cause of unexplained infertility and fatigue.
Homocysteine: An elevated level (> 7-8 µmol/L) suggests a deficiency in B12, B6, or Folate and indicates poor methylation (detoxification) capacity.
3.5 Genetics: The MTHFR Mutation
The Test: Genotyping for the MTHFR gene (C677T and A1298C variants).
The Mechanism: The MTHFR enzyme converts Folic Acid (synthetic) and food folate into Methylfolate (5-MTHF), the active form required for DNA replication and preventing neural tube defects. Individuals with this mutation (heterozygous or homozygous) have reduced enzyme efficiency (down to 30-70%).
The Implication: Women with this mutation may need to avoid synthetic folic acid and instead take methylated folate (5-MTHF) in their prenatal vitamins to ensure adequate levels and prevent the buildup of toxic homocysteine.
4. Nutritional Strategy: The Indian Functional Fertility Diet

Nutrition is the bedrock of the Arka Anugraha philosophy. However, generic Western advice like “eat the Mediterranean diet” often fails in the Indian context due to cultural preferences and food availability. The goal is to adapt functional nutrition principles to the Indian kitchen—moving away from a carb-heavy, refined-grain diet toward a nutrient-dense, whole-food protocol.
4.1 The Core Principles: The “Fertility Plate”
- Blood Sugar Stabilization: Every meal must blunt the insulin spike. This is achieved by never eating “naked carbs” (e.g., plain white rice or biscuits). Carbs must be dressed with Protein, Fiber, and Fat.
- Anti-Inflammatory: Reducing foods that trigger immune responses and increasing foods that quench oxidative fire.
- Nourishing the “Shukra Dhatu”: In Ayurveda, reproductive tissue (Shukra Dhatu) is the final tissue to be nourished, requiring the essence of all food. Therefore, the diet must be rich and building (Ojas-building).
4.2 The Functional Indian Pantry
Food Category | Functional “Superfoods” | Why It Matters for Fertility |
Healthy Fats | A2 Cow Ghee, Coconut Oil, Soaked Almonds, Walnuts, Sesame Seeds (Til) | Steroid hormones (Estrogen, Progesterone, Testosterone) are made from cholesterol. Ghee is revered in Ayurveda for nourishing deep tissues and carrying medicinal properties to cells. Walnuts provide Omega-3s for inflammation control. |
Quality Proteins | Moong Dal, Paneer (if dairy tolerant), Lentils, Chickpeas (Chana), Eggs (Desi), Lean Chicken/Fish | Proteins are the building blocks of the embryo. Plant proteins like beans/lentils are associated with lower risks of ovulatory infertility. |
Complex Carbs | Red Rice, Foxtail Millet, Jowar, Ragi, Quinoa, Sweet Potato (Shakarkandi) | These have a lower glycemic index than white rice/maida. They are high in fiber, which binds to excess estrogen in the gut and removes it. |
Spices | Turmeric (Haldi), Cumin (Jeera), Fenugreek (Methi), Saffron (Kesar), Cardamom | Turmeric (Curcumin) is a potent anti-inflammatory. Fenugreek supports insulin sensitivity and hormonal balance. Saffron is traditionally used to improve blood flow to the uterus. |
Leafy Greens | Moringa (Drumstick leaves), Spinach (Palak), Methi leaves, Mustard greens (Sarson) | Moringa is an Indian superfood, incredibly rich in iron, calcium, and antioxidants. Greens provide natural Folate (B9). |
Antioxidants | Amla (Gooseberry), Pomegranate, Guava, Berries | Amla is one of the richest sources of Vitamin C, vital for progesterone production and sperm health. Pomegranate improves blood flow. |
4.3 Sample “Fertility Friendly” Indian Meal Plan
- Early Morning: Warm water with lemon or soaked fenugreek water (for insulin sensitivity).
- Breakfast: Vegetable Upma made with Rava or Millets + a side of coconut chutney (fat) + a boiled egg or sprout salad (protein). Avoid plain toast/biscuit/chai..
- Lunch: Brown rice or Jowar Roti + Lauki (Bottle gourd) Sabzi + Yellow Dal + A generous serving of Ghee.
- Snack: A handful of soaked walnuts and almonds + a fruit like Guava (Vitamin C).
- Dinner: Moong Dal Khichdi with spinach + Curd/Buttermilk (Probiotics). Dinner should be lighter and eaten early (by 8 PM) to support circadian rhythm.
4.4 Foods to Limit or Avoid
- Trans Fats (Vanaspati/Dalda): Commonly found in street foods, fried snacks (namkeen), and commercial biscuits. These create “rigid” cell membranes, making it harder for insulin to work and for sperm to penetrate the egg.
- Refined Sugars & Maida: White bread, pasta, pizza bases, and excessive Indian sweets (Mithai). These cause rapid insulin spikes, disrupting ovulation.
- High-Mercury Fish: While fish is healthy, large predatory fish (Shark, Swordfish, King Mackerel) contain mercury, a neurotoxin that can damage the fetal brain. In India, local river fish or smaller sea fish (like Sardines/Mackerel) are safer choices.
- Raw Papaya: Contains latex and papain, which can stimulate uterine contractions. While ripe papaya is debatable, most Indian elders and doctors advise avoiding raw/semi-ripe papaya during conception and pregnancy as a precaution.
Plastics: Avoid carrying hot curries in plastic tiffin boxes or drinking from hot plastic bottles. Heat causes BPA and phthalates to leach into the food, acting as endocrine disruptors.
5. Lifestyle Optimization: "Cleaning the Soil"

In the Arka Anugraha philosophy, lifestyle is not secondary to medicine; it is medicine. Epigenetics teaches us that our genes load the gun, but our environment pulls the trigger. Preconception care is about creating an environment that signals “safety” to the body.
5.1 Environmental Detoxification (The Toxin Checklist)
We live in a chemical soup. Endocrine Disrupting Chemicals (EDCs) are substances in the environment that mimic natural hormones (like estrogen) or block them, causing chaos in the reproductive system.
- Kitchen Detox: Replace non-stick (Teflon) pans, which can release PFOA, with traditional Cast Iron (Tawa/Kadhai) or Stainless Steel. Replace plastic storage containers with glass or steel.
- Personal Care: Many creams, shampoos, and fragrances contain Parabens and Phthalates. These are known reproductive toxins. Switch to natural, fragrance-free alternatives.
- Pesticides: Indian produce can have high pesticide residue. Wash all vegetables thoroughly. Soaking them in salt water or a vinegar solution for 20 minutes can remove significant surface residue. Peel fruits/vegetables where possible.
- Air Quality: Indoor air pollution in Indian cities can be high. Use HEPA air purifiers in the bedroom and introduce air-purifying plants like Snake Plant or Spider Plant.
5.2 Sleep: The Hormonal Reset
Sleep is when the body repairs DNA. The hormone Melatonin, released during sleep, is not just for sleep; it is a powerful antioxidant that is found in high concentrations in the follicular fluid surrounding the egg, protecting it from damage.
- The Goal: 7-9 hours of quality sleep in total darkness.
- The Tactic: Implement a “Digital Sunset.” The blue light from phones and TVs suppresses melatonin. Turn off screens 90 minutes before bed.
5.3 Stress Management: The Cortisol-Progesterone Steal
Biologically, the body prioritizes survival over reproduction. The precursor hormone, Pregnenolone, is used to make both Cortisol (stress hormone) and Progesterone (pregnancy hormone). Chronic stress causes the “Cortisol Steal,” where the body diverts resources to make cortisol, leaving insufficient progesterone to support a pregnancy.
- Arka’s Approach: The hospital integrates wellness therapies. Practices like Yoga (specifically restorative poses like Supta Baddha Konasana), Meditation, and Pranayama (deep breathing) are clinically proven to lower cortisol. Dr. Gaurang’s holistic approach often involves addressing the “mindset” of the patient.
5.4 Exercise: The Goldilocks Zone
- Too Little: Sedentary behavior worsens insulin resistance.
- Too Much: Excessive High-Intensity Interval Training (HIIT) or marathon running can be perceived by the body as physical stress, potentially shutting down ovulation (Hypothalamic Amenorrhea).
Just Right: Moderate activity. Brisk walking, swimming, or specific Fertility Yoga for 30-45 minutes daily improves blood flow to the pelvic organs without spiking stress hormones.
6. The Male Factor: Sperm Optimization
It takes two to tango. Sperm counts have declined globally by over 50% in the last 40 years. Men must be equal partners in the preconception preparation.
6.1 Nutritional Support for Sperm
Sperm cells are uniquely vulnerable to oxidative stress because their plasma membranes are rich in polyunsaturated fatty acids. They need a shield of antioxidants.
- Zinc: The “Male Mineral.” Essential for testosterone production and sperm count. Sources: Pumpkin seeds, chickpeas, meat.
- Selenium: Critical for sperm morphology (shape). Sources: Brazil nuts, chicken, eggs.
- CoQ10 (Ubiquinol): The “battery” of the cell. It concentrates in the mid-piece of the sperm, providing the energy (ATP) needed for motility (swimming). Levels decline with age.
- Lycopene: A potent antioxidant found in cooked tomatoes and watermelon, shown to improve sperm structure.8
6.2 The “Cooling” Protocol
Spermatogenesis works best at temperatures 2-4 degrees below body temperature.
- Avoid: Hot baths, saunas, and tight synthetic underwear.
- Laptop Hygiene: Never place a laptop directly on the lap. The heat and electromagnetic radiation can damage sperm DNA.
- Cell Phones: Avoid carrying cell phones in the front trouser pockets.
7. Supplementation: Bridging the Gap
While a nutrient-dense diet is primary, modern soil depletion and higher stress demands often necessitate supplementation. Note: Supplements should be personalized based on lab results (e.g., Ferritin levels) and under the guidance of the Arka medical team.
Nutrient | Functional Form | Purpose |
Prenatal Multi | Comprehensive | A safety net to cover micronutrient gaps. Must contain Iodine and Zinc. |
Folate | Methylfolate (5-MTHF) | Prevents neural tube defects. Methylfolate is preferred over synthetic Folic Acid for better absorption, especially in MTHFR carriers. |
Omega-3 | Fish Oil (DHA/EPA) | 1000mg daily. DHA is critical for the fetal brain and eyes. EPA reduces maternal inflammation. |
Vitamin D3 | Cholecalciferol + K2 | Dosed based on lab levels (typically 2000-5000 IU). Supports immune tolerance and hormone synthesis. |
Probiotics | Lactobacillus/Bifido | Supports gut health and prevents Bacterial Vaginosis (a risk for preterm birth). |
CoQ10 | Ubiquinol | 200-600mg. Improves egg quality (mitochondrial energy) and sperm motility. |
Myo-Inositol | Myo + D-Chiro | Particularly for women with PCOS. It improves insulin sensitivity and restores ovulation. |
8. The Timeline: A Strategic Countdown
Planning allows for a calm, stepwise approach to health.
8.1 T-Minus 3-6 Months: The Assessment Phase
- Consultation: Book with Dr. Gaurang Ramesh or Dr. Ramesh Makam at Arka Anugraha.
- Vaccines: Review immunity. If MMR or Varicella vaccines are needed, get them now. Mandatory Waiting Period: You must avoid pregnancy for 1 month (minimum) to 3 months after live vaccines.
- Dental: Gum disease (periodontitis) allows bacteria to enter the bloodstream and is linked to preterm birth. Get a deep cleaning now.
- Detox: Stop smoking, alcohol, and recreational drugs.
- Contraception: Consider stopping hormonal birth control to allow the natural cycle to regulate. Use barrier methods (condoms) in the interim.
8.2 T-Minus 1 Month: The “Go” Phase
- Folic Acid: Ensure you have been taking it daily for at least a month.
- Tracking: Start charting your cycle. Look for signs of ovulation: cervical mucus changes (egg-white consistency) or positive ovulation predictor kits (OPKs).
Labs Check: Verify that TSH is < 2.5 and Ferritin is > 30.
9. The Arka Anugraha Advantage
Located at #2, 15th Cross, 6th Phase, J P Nagar, Bengaluru, Arka Anugraha Hospital is a sanctuary for comprehensive care. It offers 24/7 accessibility and wheelchair-friendly facilities, ensuring that care is available whenever needed.
Why Choose Arka?
- Holistic Ecosystem: It houses specialized clinics for Bariatric Surgery (crucial for patients where weight is the primary fertility barrier), Advanced Laparoscopy (for fibroids/endometriosis), and Integrative Medicine under one roof.
- Expert Leadership:
- Dr. Ramesh Makam: A veteran with 35+ years of experience, ensuring that if surgical intervention is needed (e.g., removing a septum or fibroid), it is done with world-class precision.
- Dr. Gaurang Ramesh: Provides the cutting-edge Functional Medicine perspective, addressing the “invisible” metabolic and gut-health barriers to fertility.
Patient-Centricity: The hospital focuses on “patient comfort, safety, and accessibility,” creating an inclusive environment where the anxiety of fertility planning is replaced with empowerment.
10. Frequently Asked Questions (FAQ)
Q1: Do I need to see a doctor if I am young and healthy?
A: Yes. Many conditions like Thalassemia Trait, Thyroid antibodies, or Vitamin D deficiency are “silent” but can impact pregnancy outcomes. A preconception visit is about prevention, not just curing sickness.
Q2: What if I have PCOS? Can Functional Medicine help?
A: Absolutely. Functional medicine views PCOS not as a gynecological disease but as a metabolic one (insulin resistance/inflammation). By addressing diet, gut health, and nutrient deficiencies (like Inositol/Magnesium), many women can restore natural ovulation without heavy medication.
Q3: Is the Indian diet good for fertility?
A: A traditional Indian diet (whole grains, dals, vegetables, ghee) is excellent. However, the modern Indian diet (high sugar, refined flour, fried snacks) is detrimental. The key is to return to whole, unprocessed roots.
Q4: Does Arka Anugraha offer IVF?
A: Arka Anugraha specializes in Restorative Reproductive Medicine. They optimize your body to conceive naturally or to make Assisted Reproductive Technologies (like IVF) more successful if they are needed elsewhere. They handle the surgical and medical preparation that makes conception possible.
Conclusion: Your Legacy Begins Now
The journey to parenthood is not just about the destination; it is about the vessel. By taking the time to prepare—to nourish your cells, balance your hormones, and cleanse your environment—you are giving your future child the greatest gift possible: a foundation of robust health.
Arka Anugraha Hospital invites you to step into this journey with confidence, supported by the best of modern science and ancient wisdom.
Schedule Your Preconception Consultation Today:
- Location: Arka Anugraha Hospital, JP Nagar 6th Phase, Bangalore.
- Contact: +(91) 807-373-7505
- Online: arka.health
Explore Arka Recipes
Discover recipes that blend taste with health, crafted by our experts for your well-being.

Arka Diagnostics
Discover groundbreaking diagnostic services exclusive to India, now available at Arka Health, Bangalore
